- Who We Help
- RegulatorsBetterDoctor® Provider Portal
Proven Provider Network Management
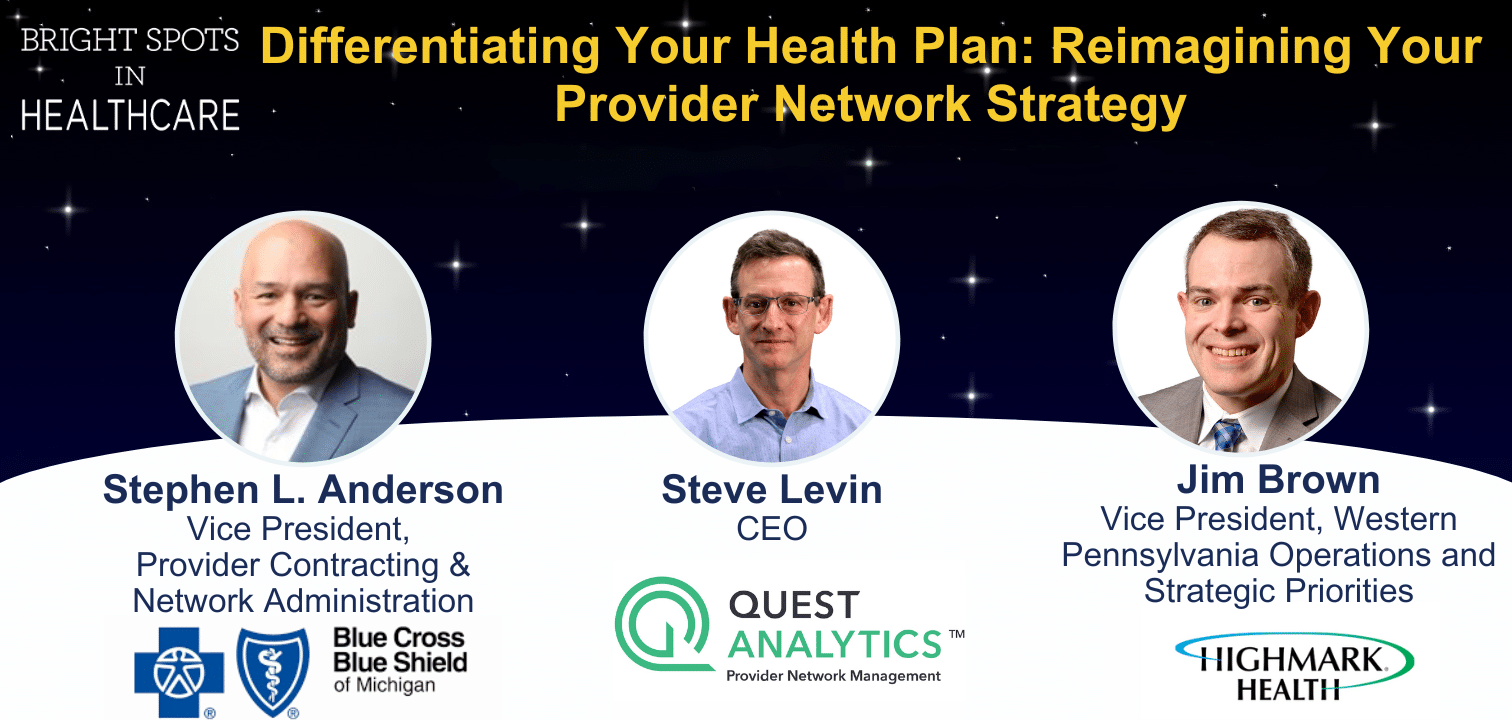
Quest Analytics® offers unparalleled provider network management solutions and services for healthcare provider networks.
- How We Help
- SolutionsBetterDoctor® Provider Portal
Explore Quest Enterprise Services® (QES®) for integrated solutions for your healthcare provider network management.
- About Us
- We Are HiringAbout Us
We're Hiring
We’re Hiring. If You’re Looking To Use Your Talents To Make A Difference In The Lives Of Healthcare Consumers – We Want To Hear From You.
- Resources
- Featured Resource Hubs
- Who We Help
- RegulatorsBetterDoctor® Provider Portal
Proven Provider Network Management
Quest Analytics® offers unparalleled provider network management solutions and services for healthcare provider networks.
- How We Help
- SolutionsBetterDoctor® Provider Portal
Explore Quest Enterprise Services® (QES®) for integrated solutions for your healthcare provider network management.
- About Us
- We Are HiringAbout Us
We're Hiring
We’re Hiring. If You’re Looking To Use Your Talents To Make A Difference In The Lives Of Healthcare Consumers – We Want To Hear From You.
- Resources
- Featured Resource Hubs