Quest Enterprise Services™ (QES™)
QES Adequacy
COMPLY, COMPETE AND GO FROM ADEQUATE TO EXCELLENT
Elevate your network beyond compliance with Quest Enterprise Services™ (QES™) Adequacy. Our comprehensive resources empower you to enhance member experiences and forge a network that stands out in the competitive landscape.
QES Adequacy
Your comprehensive solution for network compliance management
Quest Enterprise Services™ (QES™) Adequacy is a network compliance SaaS solution that makes it easy to measure, manage, monitor, and model network adequacy and network performance. Extending visibility to all lines of business, QES Adequacy provider network management software empowers your team to collaborate, streamlines and automates compliance processes, and helps you make informed decisions to differentiate your network. Out-maneuver your competition, expand your network, and take the complexity out of your compliance efforts, all through one intuitive platform.
Compliance Assurance
Maintain network adequacy and adhere to regulatory requirements—relying on the same data and tools regulators depend on.
Elevated Member Experience
Retain and grow your member population by ensuring your members have the right access to care, when and where they need it.
Network Management Efficiency
Build and expand your networks with adequacy analysis and insights that allow you to optimize operations in existing markets and leverage your current network to meet adequacy in new markets.
Proven ROI
Boost efficiency while capitalizing on new market opportunities with a single enterprise-wide platform.
- Popular Features
- Use Cases
- Related Solutions
- Related Resources
Popular Features
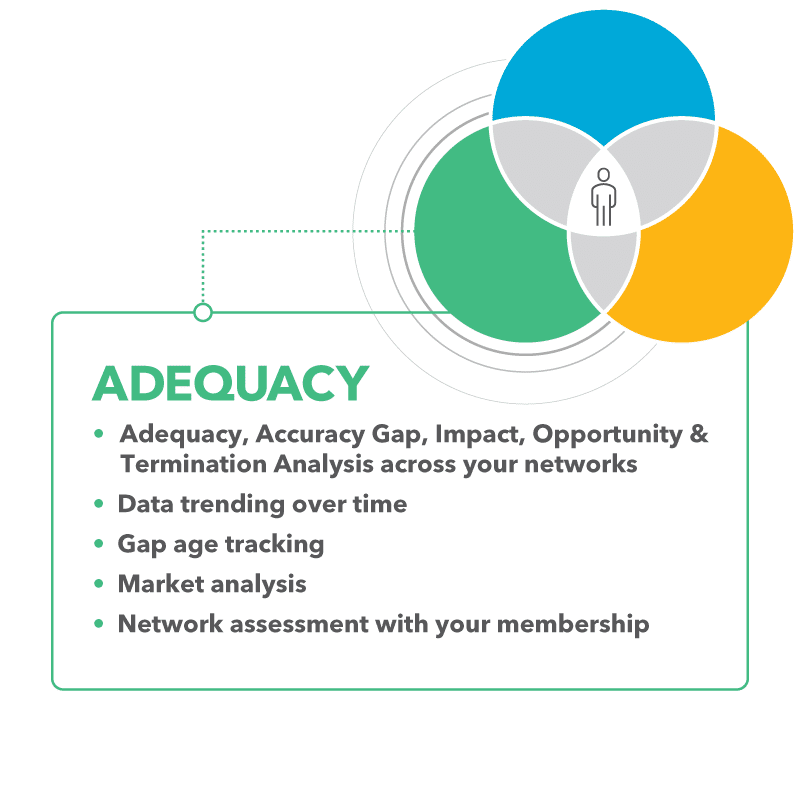
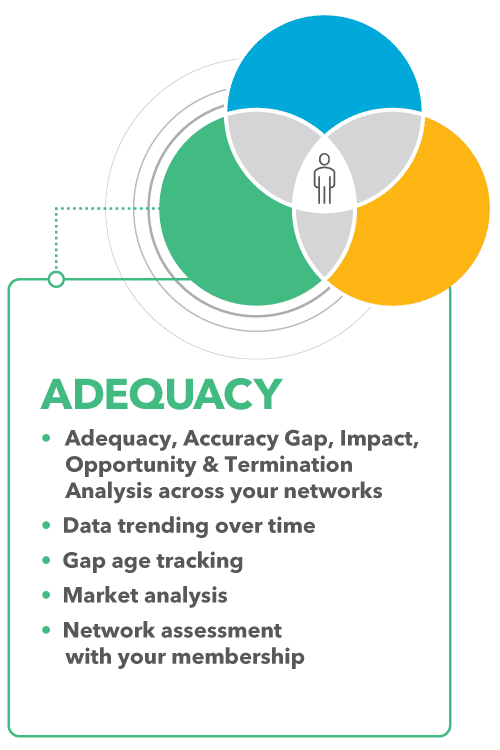
Explore the top features of QES Adequacy – your keys to managing networks with precision across all lines of business, streamlining organization efficiency, ensuring seamless member access, and minimizing regulatory risks.
Gap Management, Trending and Resolution
Increase visibility into network adequacy gap trends, identify specialties with compliance issues, and monitor the status of gaps and the time needed for resolution. With this insight, you can proactively address network gaps.
Impact Analysis
Gain valuable insights into provider availability within the market, across different lines of business, and the impact on your network adequacy based on geographic location and specialty.
Network Adequacy Templates
Streamline your path to compliance with our regulator-endorsed Network Adequacy Templates. Our deep partnerships with regulators provide you the ultimate toolkit to evaluate and oversee your networks, mirroring the scrutiny of regulators themselves—just like having the answers before the test. Access our robust collection of ready-made and customizable federal and state network adequacy templates, including the pre-built CCIIO QHP template.
Provider Recruitment Tracking
Pinpoint providers to recruit to fill gaps, and track recruitment efforts throughout the year, streamlining your adequacy compliance efforts while supporting exception or justification requests.
Time and Distance Calculation Methodologies
Select the optimal method needed for your network adequacy analysis – including straight-line distance, geographic distance, and estimated travel distance – to comply with specific requirements.
Gap Density Mapping
Enhance your understanding of network gaps by visualizing their status geographically, enabling you to identify areas that require attention to improve network adequacy.
Compliance Monitoring
Streamline, measure, and monitor network adequacy scores across lines of business. Easily understand the source of compliance issues and the capacity of market providers to resolve it with color-coded highlights at the specialty and geography level.
Provider Network Adequacy Analysis
Identify whether your network has a sufficient number and type of servicing providers based on QES analysis that calculates and assesses time, distance, and provider ratio requirements across five different geographic county classifications.
QES Adequacy in Action
QES Adequacy supports health plans, including specialty plans, health systems and regulators in their work to ensure that members have the right access to the right healthcare at the right time.
Payer Networks: Network Management Across Lines of Business
Provider networks can take charge of network management across all lines of business, including Medicare Advantage, Medicaid, Marketplace, and Commercial. Gain a competitive edge by analyzing, managing, and reporting on provider network adequacy and provider data accuracy from a single platform, across the entire organization.
Health Systems: Evaluate Adequacy Coverage Across Payers
Operate with complete visibility into your participation, access, and adequacy across all payers in all service areas. Leverage your information and insights to gain a competitive advantage, particularly during contract negotiations with existing and prospective payer organizations.
Specialty Plans: Increase Data Transparency & Streamline Compliance
Strengthen plan partnerships, secure government program contracts, and expand market presence with superior network management. Improve data transparency and cross-team collaboration, while maintaining compliance.
Regulators: Shaping the Future of Healthcare
Leverage QES Adequacy solutions, services, and expertise to drive the evolution of network adequacy standards, improve provider directory accuracy, monitor compliance with health plan requirements, and provide transparency and consumer protections in the marketplace.
Related Solutions
Unlock the full potential of your network with our suite of related solutions. Designed to integrate and complement QES Adequacy, these solutions work in tandem and further accelerate your work to boost efficiency and build high-performing networks.
Enhance exception narratives and expedite reports by using zip code summaries and the next closest provider allowing you to save time and help regulators better understand the justification for the network adequacy exception.
Model and assess your network using your member data and membership measured by regulators. You can also prioritize filling deficiencies based on the amount of membership at risk.
Simplify large-scale provider network analysis and reporting with three powerful tools. Create value-based or tiered networks with better modeling while improving your strategic understanding of how current and future provider contracts impact your network adequacy.
Leverage executive-level dashboards that provide network adequacy insights across your lines of business and networks, allowing leadership and teams to make strategic decisions focused on network adequacy.
Improve your network performance with claims data, including volume of claims, payer mix, cost, and quality, as well as top procedures and conditions embedded into the QES platform to help eliminate ghosts, select the best provider to fill network gaps, and assist with expansion efforts.
Leverage a continuously updated database of provider information as a reference file against your network information, supporting your network adequacy and performance efforts and outcomes.
Discover More
Dive into additional resources for more information and valuable insights.
DELIVER ON TOMORROW’S GOALS BY PLANNING TODAY
We are committed to assisting you in your quest to achieve the Quadruple Aim – lowering costs and ensuring high quality of care while empowering patient and clinician experiences with actionable insights.
Schedule a consultative session with one of our experts to discuss and determine your strategy.

Start a Conversation Today!