For Dental and Vision Networks
PROVIDING SMARTER MANAGEMENT FOR TODAY’S DENTAL AND VISION PLANS
Quest Analytics helps 90% of all healthcare networks deliver differentiated member and patient experiences. Let us show you how.

THE LEADING PROVIDER NETWORK MANAGEMENT PARTNER
Quest AnalyticsTM helps America’s leading dental and vision plans measure, manage and monitor network performance across all business lines.
Our Quest Enterprise ServicesTM links network adequacy and provider directory accuracy thereby reducing regulatory risk for both measures, while allowing you to integrate actionable data and insights within your workflow, including credentialing, directories, contracting, claims and more.
NETWORK ADEQUACY AND PROVIDER ACCURACY FOR YOUR DENTAL AND VISION NETWORKS
With 30 years experience in analyzing networks, we’ve developed the industry standards for network adequacy used by every insurance company in the U.S. Now within our SaaS based Quest Enterprise Services, you are able to quickly and easily measure, manage and monitor all your specialties for government or commercial programs.

RESPOND CONFIDENTLY TO RFPS
Quest Enterprise Services gives you a competitive advantage when responding to RFPs by allowing you to show your network’s differentiators based on each client’s specialty utilization: by market share, availability, capacity and provider directory accuracy. Not to mention having the ability to demonstrate total market accessibility (reducing out of network utilization) and accuracy analytics (reducing surprise billings).
RESPOND CONFIDENTLY TO ACCREDITATION REQUESTS
Demonstrating consistency in how you measure, manage and monitor your network’s adequacy and provider directory accuracy is a key component to accreditation. Quest Enterprise Services helps you respond to accreditation agency requests, such as NCQA or URAC, by providing you with the ability to demonstrate your network’s performance over time.
QUEST DENTAL AND VISION SERVICES
Provide access to the tools and insights your team needs to work more intelligently and more proactively.
TO HELP YOU ENSURE YOUR MEMBERS HAVE ADEQUATE ACCESS TO CARE, OUR SERVICES INCLUDE:
1. Competitive Advantage RFPs
Provide brokers and consultants a real-time view into the adequacy of your commercial network and accuracy of your provider data on a ongoing basis.
2. Provider Data Management Services
Validate your provider network data, while tracking and trending your progress over time.
3. Market Comparisons
Understand the depth of your network and your market share compared to the total availability of providers by specialty.
4. Membership Analysis
Model and assess your network using your own member data, in addition to a beneficiary or census file supplied by a regulator. Also, prioritize filling deficiencies based on the amount of membership at risk.
5. Network Performance Trending
Respond to accreditation agency requests, such as NCQA with confidence by demonstrating an ongoing process and providing a real-time view into network performance over time.
6. Adequacy Services
Measure, manage and monitor your network adequacy score in real-time, including the ability to understand how current and future provider contracts impact your network adequacy. Utilize additional metrics on network/prospect providers that you want, such as quality, utilization fields or cost & efficiency data.
7. Accuracy Services
Understand what’s right, wrong and missing within your provider data enabling you to remediate issues, manage any potential impact on your network adequacy and track performance over time.
8. Impact Analysis Services
Fill your gaps more efficiently. View what providers are available in the Market as well as within your other lines of business and their impact on your network adequacy by geography and specialty.
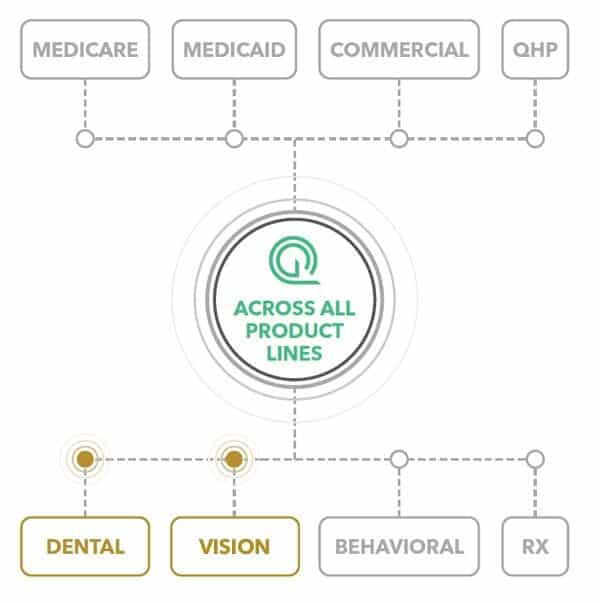
ADEQUACY + ACCURACY IN ONE PLATFORM
By running all of your networks through a single provider network management platform, you’ll gain a better understanding of the strength of your network and the impact of your providers across business lines. You’ll create cross-departmental efficiencies, cut costs and have a realtime lens into how your network compares to the market.
Discover More
Dive into additional resources for more information and valuable insights.
National Vision Care Administrator Enhances Provider Network and Expands Health Plans with Quest Analytics
Discover how a National Vision Care Administration achieved a 15+ Health Plan Expansion and a reliable provider data accuracy process with Quest Analytics.
Provider Data Accuracy Resource Hub
Provider Data Accuracy Resource Hub New Health Policy Episode Get ready for 2025 with the latest insights on major health policy changes! Join Kate Deiters and Zach Snyder as they...
Medicare Advantage and Medicaid Resource Hub
CMS Medicare Advantage and Medicaid Resource Hub Discover the latest insights and proven provider data management tips for CMS compliance. Our expanding collection of resources is here to help you...
Marketplace QHP Resource Hub
QHP MARKETPLACE RESOURCES Essential resources for issuers applying for QHP Certification to participate in the Marketplaces. Explore our growing library to find the latest news, tips, and support. New Health...
Increasing Provider Data Accuracy Oversight Across Healthcare Markets
Increasing Provider Data Accuracy Oversight Across Healthcare Markets Stay Informed with the Latest Regulatory Updates and Trends Federal and state regulators are actively amending network adequacy and provider directory accuracy...
5 Trends To Watch in the Dental Benefits Industry
What’s the latest in the dental benefits industry? We’re here to fill you in on the five trends that are shaping dental plan design. From revenue strategies to improving access...
Provider Data and Reporting Trends to Know in 2024
Data and analytics are working their magic, transforming the way we manage provider networks. From evolving technology to regulations, changes are happening all around us. Which begs the question: What...
National Vision Care Administrator Enhances Provider Network and Expands Health Plans with Quest Analytics
Discover how a National Vision Care Administration achieved a 15+ Health Plan Expansion and a reliable provider data accuracy process with Quest Analytics.
Provider Data Accuracy Resource Hub
Provider Data Accuracy Resource Hub New Health Policy Episode Get ready for 2025 with the latest insights on major health policy changes! Join Kate Deiters and Zach Snyder as they...
Medicare Advantage and Medicaid Resource Hub
CMS Medicare Advantage and Medicaid Resource Hub Discover the latest insights and proven provider data management tips for CMS compliance. Our expanding collection of resources is here to help you...
Marketplace QHP Resource Hub
QHP MARKETPLACE RESOURCES Essential resources for issuers applying for QHP Certification to participate in the Marketplaces. Explore our growing library to find the latest news, tips, and support. New Health...
Increasing Provider Data Accuracy Oversight Across Healthcare Markets
Increasing Provider Data Accuracy Oversight Across Healthcare Markets Stay Informed with the Latest Regulatory Updates and Trends Federal and state regulators are actively amending network adequacy and provider directory accuracy...
5 Trends To Watch in the Dental Benefits Industry
What’s the latest in the dental benefits industry? We’re here to fill you in on the five trends that are shaping dental plan design. From revenue strategies to improving access...
Provider Data and Reporting Trends to Know in 2024
Data and analytics are working their magic, transforming the way we manage provider networks. From evolving technology to regulations, changes are happening all around us. Which begs the question: What...
National Vision Care Administrator Enhances Provider Network and Expands Health Plans with Quest Analytics
Discover how a National Vision Care Administration achieved a 15+ Health Plan Expansion and a reliable provider data accuracy process with Quest Analytics.
Provider Data Accuracy Resource Hub
Provider Data Accuracy Resource Hub New Health Policy Episode Get ready for 2025 with the latest insights on major health policy changes! Join Kate Deiters and Zach Snyder as they...
Medicare Advantage and Medicaid Resource Hub
CMS Medicare Advantage and Medicaid Resource Hub Discover the latest insights and proven provider data management tips for CMS compliance. Our expanding collection of resources is here to help you...
Marketplace QHP Resource Hub
QHP MARKETPLACE RESOURCES Essential resources for issuers applying for QHP Certification to participate in the Marketplaces. Explore our growing library to find the latest news, tips, and support. New Health...
Increasing Provider Data Accuracy Oversight Across Healthcare Markets
Increasing Provider Data Accuracy Oversight Across Healthcare Markets Stay Informed with the Latest Regulatory Updates and Trends Federal and state regulators are actively amending network adequacy and provider directory accuracy...
5 Trends To Watch in the Dental Benefits Industry
What’s the latest in the dental benefits industry? We’re here to fill you in on the five trends that are shaping dental plan design. From revenue strategies to improving access...
Provider Data and Reporting Trends to Know in 2024
Data and analytics are working their magic, transforming the way we manage provider networks. From evolving technology to regulations, changes are happening all around us. Which begs the question: What...
SOLVE YOUR PROVIDER DIRECTORY ACCURACY CHALLENGES TODAY
Our team is ready to help you address the challenges provider data presents. We want to help you take your member experiences to the next level and avoid regulatory risks, like audits, and meet the mandates around surprise billing.
Contact us today to book a strategy session to understand and provide guidance to limit your exposure.