Quest Enterprise Services® (QES®)
Advanced Decision Applications
Power Up Your Provider Network Adequacy Management
Discover innovative tools that provide exceptional data insights and boost productivity, empowering you to reduce network adequacy compliance risks, and make strategic decisions with confidence.
Quest Enterprise Services® Advanced Decision Applications
Your solution for unparalleled network insights and productivity
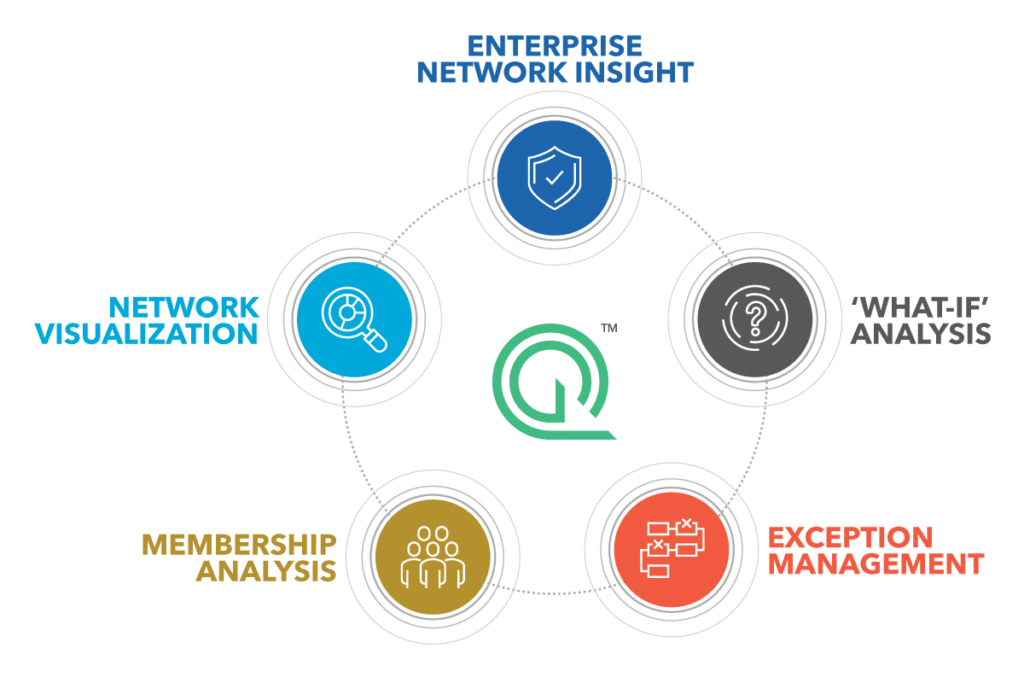
The Advanced Decision Applications suite in Quest Enterprise Services® (QES®) is here to make provider network management simpler and more efficient. With tools dedicated to scenario modeling, handling network adequacy exceptions and justifications, and advanced membership analysis, your team can address business needs effectively.
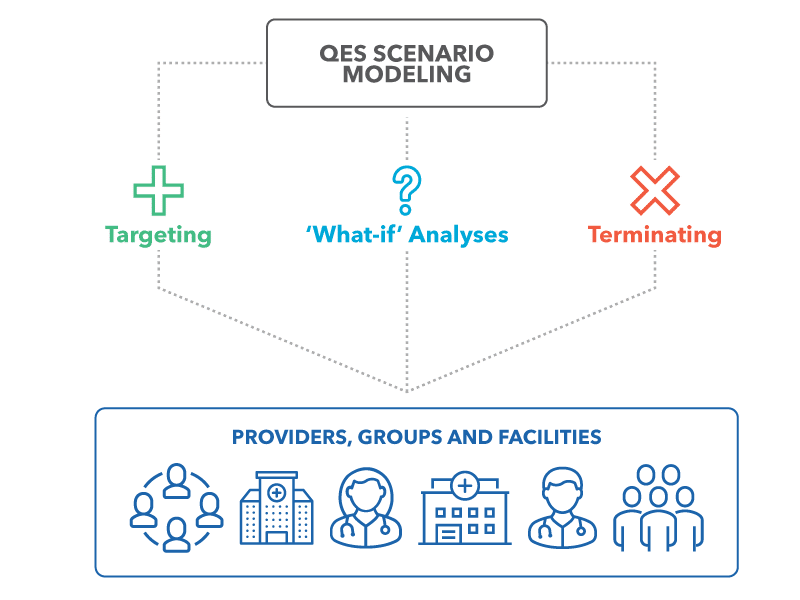
Quest Enterprise Services® Scenario Modeling for Provider Data Management at Scale
Managing large groups of providers or facilities individually can be a tedious and inefficient task, particularly when it stretches across multiple business lines. But what if there was a better way?
Quest Enterprise Services® Scenario Modeling provides you with the tools needed to navigate large and complex provider network changes. You’ll be able to conduct comprehensive ‘what-if’ analyses, evaluate the effects of targeting or terminating numerous providers and facilities, and adjust your strategies for optimum outcomes.
Volume Reporting simplifies generating provider network reports. This enhanced efficiency, combined with the valuable insights gained from these reports, facilitates the development of more effective strategies.
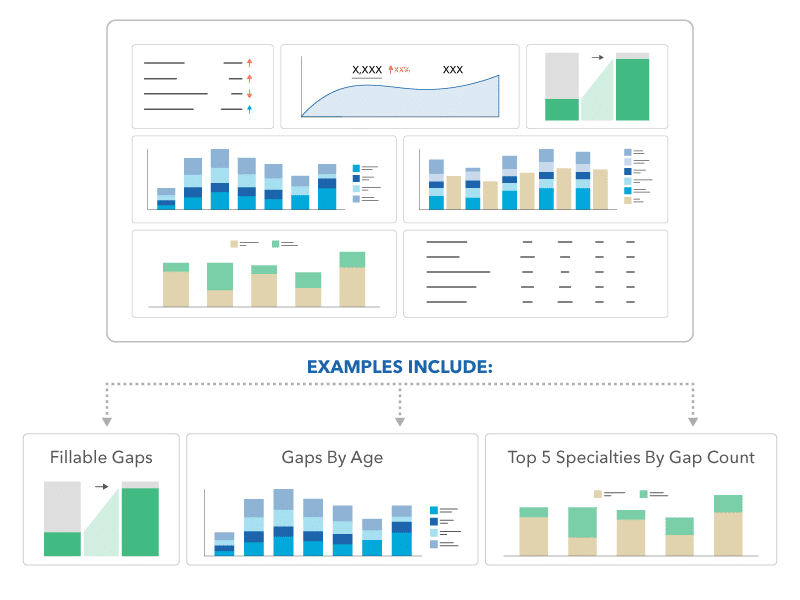
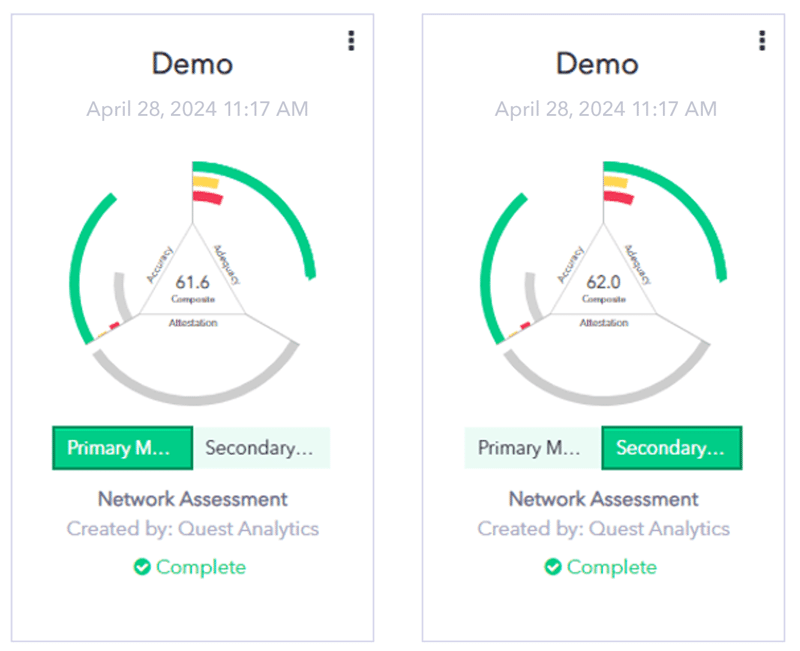
Quest Enterprise Services® Enterprise Compliance Dashboard for Enhanced Network Visibility
Increase your network visibility with the Quest Enterprise Services® Enterprise Compliance Dashboard. Manage network changes and comply with requirements effortlessly with centralized, real-time analysis and multiple viewing options. Streamline workflows, reduce redundant tasks, and make informed decisions with intuitive visuals, empowering your team to meet network adequacy goals confidently.
With the Quest Enterprise Services® Enterprise Compliance Dashboard, you can:
- Gain Multiple Perspectives: View your network by county, line of business, specialty, and exceptions.
- Pinpoint Network Adequacy Needs: Identify gaps, network changes, exclusions, and exceptions across all lines of business.
- Streamline Workflows: Reduce time and resources spent on external dashboards and redundant tasks.
- Enhance Decision-Making: Use sophisticated visualizations to elevate and expedite leadership actions.
Quest Enterprise Services® Network Adequacy Exceptions
Wish you could expedite your network adequacy exception request process? It’s now possible! The Quest Enterprise Services® Exceptions Package is designed to save you valuable time and simplify finding the facts that support your exception requests to regulators.
With Quest Enterprise Services® Exceptions, you get:
- Zip Code Summaries – Easily identify members who don’t have access to care within the regulatory standard at a zip code level.
- Next Closest Network Provider – Quickly find the distance or time to the next closest network provider.
- Next Closest Market or Prospect Provider – Identify the next closest Market or Prospect Provider between members that do not have access and the Next Closest Network Provider within the established standard to provide for exception requests.
- Sources – Utilize the populated list within QES to easily select your sources from a drop-down list and export it for the required form.
Quest Enterprise Services® Membership Analysis
Evaluating your provider network based on federal or state beneficiary or census data is important for network adequacy compliance. You also want to evaluate network coverage for your members. Quest Enterprise Services® Membership allows you to upload your membership files and run comparative analyses—all in one place.
- Membership Analysis – Run analyses based on your custom membership distribution file.
- Membership Compare – Compare analyses across membership distribution data or with the sample beneficiary file.
- Membership Risk – See the number of members at risk due to any deficiencies, or gaps, in your provider network at the state and county levels.
- Membership Binding – Assign a specific subset of your membership to a given specialty.
Discover More
Dive into additional resources for more information and valuable insights.
Ready to Elevate Your Network Management?
Discover how Quest Enterprise Services® can transform your provider network management and elevate your operational efficiency. Connect with us today to get started.

Start a Conversation Today!