Payers and Health Plans
Empowering Healthcare Payers with Advanced Provider Network Management
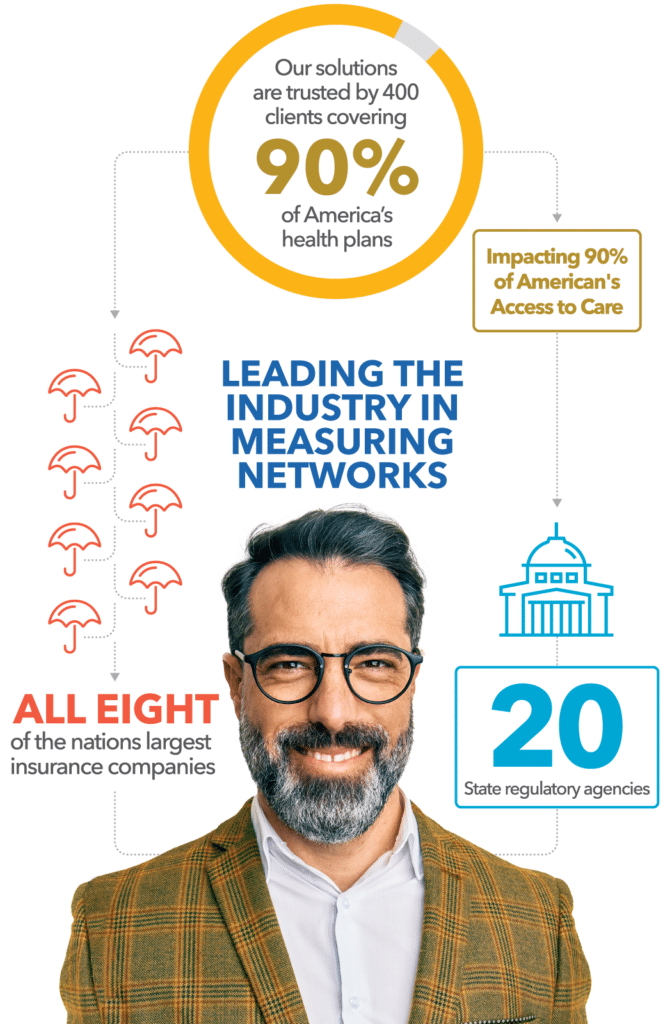
Your Strategic Partner in Provider Network Management
Today, creating access to care for your members is no longer accomplished by regulatory compliance alone. It’s about delivering high-quality, differentiated, and competitive networks that also address the unique needs and health equity considerations of your members. Quest Enterprise Services® (QES®), our self-service SaaS-based provider network management and decisioning platform, gives you a competitive edge by allowing you to measure, manage, monitor, and model your provider network adequacy, performance, and provider data accuracy across your entire organization and all lines of business. It does all that in a single solution—something no one else can offer.
Maintaining Regulatory Compliance
Provider Directory Data Accuracy
Enhance provider data accuracy with regular checks against trusted sources like NPPES, OIG, machine learning, and our BetterDoctor® Exchange. We help you promote verified data, demote unverified, fix inaccuracies, and note changes for quality assurance.
Workflow Efficiency Across all Lines of Business
Streamline your organization’s processes with tools and insights that help eliminate cross-departmental silos and unite your network management, performance, compliance across all lines of business — giving your team an efficiency boost, while improving your overall member experiences with measurable ROI.
Unique Data Analytics & Insights
Boost your strategic goals by harnessing unparalleled insights from our exclusive data. Our insights stem from our proprietary data – network files submitted by payers and then validated by regulators, reflecting a true state of the network. By enriching this data with BetterDoctor® attestations, affiliations, and claims information, we unlock unique insights into network adequacy and performance, helping you understand the competitive landscape and build differentiated networks.
Supporting All Healthcare Lines of Businesses
We are your partner in optimizing provider networks for commercial health insurance plans. We understand the vital role that a strong network plays in delivering quality healthcare to insured populations. That is why we have developed tools within QES designed specifically for you: the forward-thinking commercial insurance market professionals committed to staying ahead and delivering the best outcomes for your members. Our proven provider network management solutions empower you to take your network from adequate to competitive, ensuring that you can meet the needs of your insured population and stay ahead in this ever-evolving industry.
Our long-standing partnership with the Centers for Medicare & Medicaid (CMS) equips Medicare Advantage and Medicare-Medicaid Plans with innovative, automated solutions and templates designed to streamline network management, elevate operational efficiency, and ensure compliance with CMS Network Adequacy and Provider Directory requirements.
Our platform provides essential insights for teams focused on network optimization, provider recruitment, market growth, network submissions, network applications, and Triennial Network adequacy audits. With multiple viewing options and automatic data analysis, it promotes team collaboration and regulatory compliance. This allows Medicare Advantage and Medicare-Medicaid Plans to strategically plan service area expansions and improve the member experience.
We provide Medicaid Plans with innovative, data-driven network management solutions. Our platform uniquely measures network adequacy and provider data accuracy simultaneously, ensuring compliance and operational excellence. Say goodbye to interpreting each different state Medicaid template, all with different and unique requirements, and hello to time savings by leveraging our pre-built Medicaid templates. By leveraging our advanced tools, Medicaid plans can efficiently address gaps in provider networks and directories, leading to improved compliance, enhanced member experiences, and a competitive edge in the healthcare market.
We offer sophisticated, targeted solutions designed to streamline provider network management for Qualified Health Plans (QHPs). Our services are tailored to support health insurance issuers in efficiently navigating complex aspects such as network adequacy compliance, provider data accuracy, and QHP certification.
With our ready-made templates and custom solutions, issuers on the Federally-facilitated Exchange, the State-Based Exchanges and the State-based Exchanges on the Federal Platform (SBE-FPs), can easily monitor network adequacy, support provider recruitment, evaluate network expansion, identify and remediate network deficiencies, and maintain the highest standards of provider data accuracy.
Transforming Ancillary Healthcare with Quest Analytics
Quest Analytics simplifies healthcare management, offering solutions for Dental Plans, Vision Plans, Health Systems, and Behavioral Health. We address challenges National and Regional Payers face, from regulatory compliance to member experience enhancement. Our tools help balance quality and cost, align with market goals, and maintain competitive differentiation. Partner with us to navigate the healthcare landscape and redefine healthcare management.
Enhancing Vision Plan Efficiency
Streamlining Health System Operations
Advancing Behavioral Health Services
"Monitoring and maintaining network adequacy on a weekly basis has been incredibly beneficial for our organization."
— Director of Network Management, Regional Health Plan
— VP of Healthcare Services, National Health Plan
— Chief Operations Officer, Ancillary Plan
"Quest Analytics innovative solutions have transformed our approach to network adequacy, enhancing our productivity."
— Senior Product Manager, National Health Plan
"Identifying impactful targets has never been easier, thanks to the intuitive design of the tools."
— Network Development Specialist, Regional Health Plan
Discover More
Dive into additional resources for more information and valuable insights.
Tune In: The Totally Adequate Podcast
Initiating conversations on the latest trends, network adequacy and provider data accuracy policy updates, and healthcare provider network management innovations.
DELIVER ON TOMORROW’S GOALS BY PLANNING TODAY
We are committed to assisting you in your quest to achieve the Quadruple Aim – lowering costs and ensuring high quality of care while empowering patient and clinician experiences with actionable insights.
Schedule a consultative session with one of our health systems experts to discuss and determine your strategy.

Start a Conversation Today!