QHP MARKETPLACE RESOURCES
Essential resources for issuers applying for QHP Certification to participate in the Marketplaces. Explore our growing library to find the latest news, tips, and support.
New Health Policy Episode
Get ready for 2025 with the latest insights on major health policy changes! Join Kate Deiters and Zach Snyder as they break down federal policy updates related to network adequacy and provider directory accuracy. Discover what’s changing and how you can start preparing for the new requirements.
- The Propose 2026 Notice of Benefit and Payment Parameters
- Managed Care Final Rule
- Mental Health Parity and Addiction Equity Act (MHPAEA) Final Rule
- CMS National Directory Pilot
- Trends for 2025
Featured Marketplace Resources
Policy Brief: PY2025 QHP Certification Marketplace Final Rule
Key Insights: PY2025 & PY2026 QHP Certification New QHP Network Adequacy Requirements Explained Discover the latest Network Adequacy and Provider Directory Accuracy Requirements for QHP Certification The rules have changed,...
Executive Summary: New Rules for PY2025 QHP Certification
Be Ready for Network Adequacy and QHP Application Changes Understanding the New QHP Certification Process Big changes are just around the corner! Network adequacy requirements for Qualified Health Plan (QHP)...
Tips for QHP Issuers: Completing the Network Adequacy Template
Successfully Submit Your Network Adequacy Data Get ahead in your QHP certification by providing the correct information. Take advantage of these six tips to successfully submit your data using the...
Watch Now: The Role of Adequate Health Networks in the Marketplace
The Role of Adequate Health Networks in the Marketplace Quest Analytics® is hosting leadership from The CMS Center for Consumer Information and Insurance Oversight (CCIIO) for a conversation about network...
HHS Notice of Benefit and Payment Parameters Latest Proposed Rule
On October 4, the Centers for Medicare & Medicaid Services (CMS) unveiled the proposed Notice of Benefit and Payment Parameters for the 2026 plan year (Proposed 2026 Payment Notice) alongside...
CMS Provider Directory Pilot: What You Need to Know
CMS Qualified Health Plan (QHP) Directory Pilot The Centers for Medicare & Medicaid Services (CMS) launched a new provider directory pilot program with the Oklahoma Insurance Department (OID). Kate Deiters...
Explore Our Latest Articles
CMS Releases Proposed Rule Impacting Medicare Advantage Organizations for Contract Year 2026
On December 10, 2024, the Centers for Medicare & Medicaid Services (CMS) released a proposed rule impacting Medicare Advantage (MA) Organizations for Contract Year 2026. This proposal introduces pivotal provisions...
FAQs: Medicare Advantage Applications and Letters of Intent
Medicare Advantage (MA) Organizations applying for initial, or service area expansion can use Letters of Intent in place of a signed contract to help meet network adequacy requirements while going...
Medicare Advantage Network Adequacy and Provider Data Accuracy Toolkit
Medicare Advantage Network Adequacy and Provider Data Accuracy Audit Toolkit Comprehensive Toolkit for Network Evaluations and Strategy Are you looking to evaluate your network and strategy in line with CMS...
Ghost Networks
Ghost Networks in Healthcare: What They Are and How To Address Them
Ghost networks have increasingly become a central topic in discussions within the healthcare sector and legislative circles. As this issue gains attention, it is crucial to understand the implications of...
How Ghost Networks Impact Health Plans and Health Systems
Health plans and health systems face significant financial challenges due to the presence of ghost providers. Keeping these providers in your data undermines the efficacy of health systems, resulting in...
Tips to Avoid the Ghost Network Trap
Ghost Networks are a significant challenge in the healthcare industry. By adopting a standard operating procedure that helps you understand which providers are truly clinically active, you can increase the...
Network Performance
The Role of Health Networks in Shaping Healthcare
Listen on: Spotify Apple Youtube Episode: The Role of Health Networks in Shaping Healthcare Date: April 3, 2024 Guests: Steve Levin, CEO, Quest Analytics | Connect on LinkedIn Subhash Seelam,...
Episode: Benchmarking for Better Networks: Optimizing Health Plan Performance
Guest on: Becker’s Healthcare Podcast Benchmarking for Better Networks: Optimizing Health Plan Performance Health plans rely on complex networks of providers to deliver care to their members. But how do...
Addressing the Top 10 Questions on Healthcare Provider Network Benchmarking
Network benchmarking and competitive analysis are essential for healthcare organizations seeking to enhance network performance, improve patient outcomes, and drive sustainable growth. As healthcare organizations confront increasing demands to deliver...
Find provider data accuracy resources, webinars, guides, and expert advice to help you stay compliant and performant.
Provider Data Management Tips & Resources
Success Stories
Outgrown Homegrown System
This MCO faced unique challenges in efficiently assessing and ensuring network adequacy and provider data accuracy for its Medicaid program.
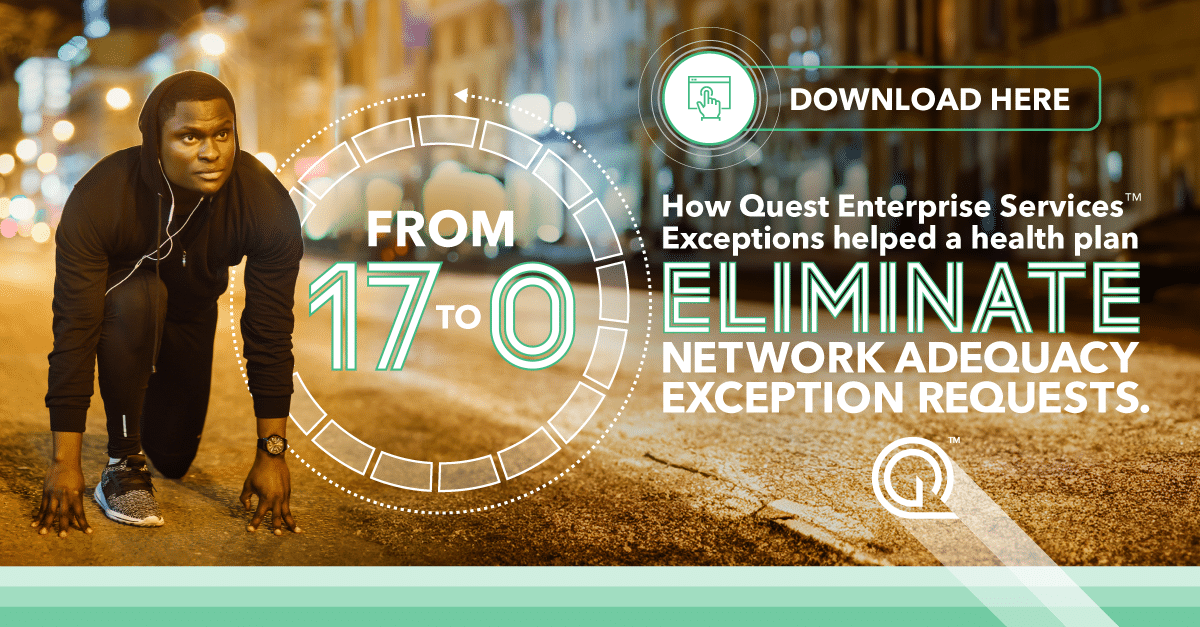
Case Study Network Adequacy Exceptions
Reducing, Expediting and Enhancing Network Adequacy Exception Requests The client was having trouble meeting network adequacy requirements in certain counties, and every year this happened, they had to file exception...
Clarity in Complexity
Delivering the Data Insights Health Systems Need to Drive Performance Gathering and analyzing data can be daunting, but Quest Enterprise Services makes it effortless. We provide you with the actionable...
Schedule Your Complimentary Strategy Session
Compliance isn’t our name, but it sure is our game! Learn how we can assist your efforts to make your provider data accurate and network adequate. Book a complimentary strategy session with a Quest Analytics expert to get started on your quest for success.