When was the last time you relied on your provider network data? Was it to prepare for a regulatory submission? Evaluate network performance? Update provider directories? Or maybe to decide whether to continue offering a specific product? No matter the reason, one factor was likely central to your outcome: provider data accuracy.
Accurate and up-to-date provider data is critical to the success of your organization—but maintaining that level of accuracy is no small task. Provider data validation plays a key role in meeting this challenge, helping keep information reliable. When done correctly, provider data validation strengthens compliance, improves operational efficiency, and enhances experiences for both members and providers.
What is Provider Data Validation?
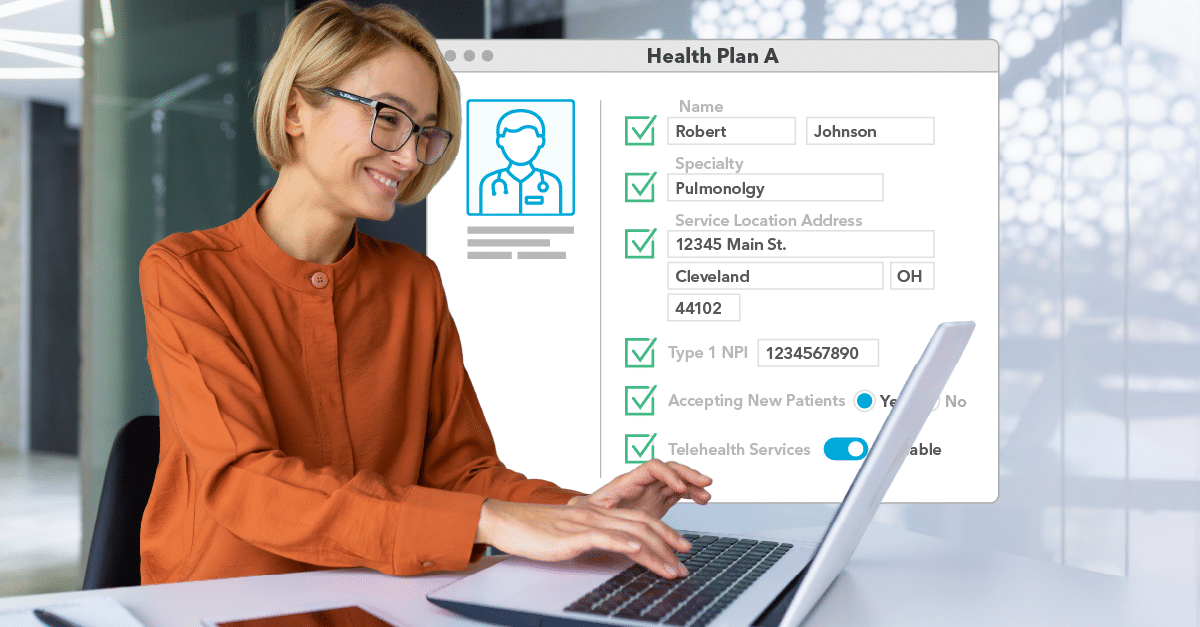
Healthcare provider data validation is the process of reviewing and confirming that the information you have on record for your contracted healthcare providers is current, correct, and complete. It includes verifying key details like contact information, practice locations, accepting new patients status, and telehealth services.
The process involves directly engaging with providers to verify their information. Once verified, the updated data is integrated across your organization’s systems and member-facing resources, like provider directories, that members rely on to make informed healthcare decisions.
What Does Provider Data Validation Involve?
- Engaging Providers: This step involves providers confirming or updating their information such as: National Provider Identifier (NPI), name, specialty, practice address, phone number, telehealth service, cultural and linguistic capabilities, and accepting new patients status.
- Updating Internal Databases and Systems: Once the data is confirmed, the next step is to make sure it’s synced across your organization’s internal databases and systems.
- Sharing Verified Information Publicly: Finally, the updated data is shared through external channels, such as provider directories, marketing materials, or regulatory network submissions and reports.
Get Your Free Provider Data Accuracy Toolkit
Take the guesswork out of compliance and operational efficiency. This free audit workbook helps you evaluate the accuracy of your provider data, identify gaps, and strengthen your processes—all in one place. Download now!
Why is Provider Data Validation Important?
Provider data touches almost every aspect of your business, and mistakes in this data can have significant consequences. Incorrect or outdated data negatively affects compliance, member satisfaction, and operational efficiency. Validating your provider data helps you avoid these risks and positions your health plan as reliable, transparent, and aligned with member needs.
Protect Your Organization by Maintaining Regulatory Compliance
Federal and state regulations mandate provider directory accuracy to help consumers access care without unnecessary obstacles. While the specific requirements vary depending on the program for example, CMS Medicare Advantage, No Surprises Act, and state-specific regulations, the consequences of failing to comply remain consistent across the board.
Noncompliance can lead to:
- Significant monetary fines
- Contract termination
- Reputational damage
These consequences create ripple effects across your organization, affecting financial stability and performance. By investing in provider data validation, you minimize these risks and demonstrate transparency and accountability to members, regulators, and stakeholders.
💡 Want to stay informed about regulatory updates that impact your network? Read our article on Network Adequacy and Provider Directory Accuracy Policy Updates for the latest insights.
Improve Member Experience and Care Accessibility
For members, provider data is often their first point of contact when seeking care. Whether they need to locate an in-network physician, confirm they’re covered, or schedule an appointment, accurate directories and resources are crucial. Incorrect information—such as outdated phone numbers or an inaccurate office address—leads to frustration and wasted time.
Even worse, repeated errors erode trust, and unhappy members may eventually switch to another health plan they believe better meets their needs. On the other hand, when provider directories are accurate, members can navigate the healthcare system without unnecessary stress, building loyalty and fostering a positive relationship with your organization.
💡 Want to learn how unvalidated provider data affects members? Read our article on The Hidden Costs of Inaccurate Provider Data to discover the wider impact.
Minimize Operational Inefficiencies
Maintaining reliable provider data also benefits your internal operations. Without proper validation processes, incorrect or outdated data can compromise network management, delay network development, and hinder network optimization, causing additional, unnecessary work for your teams. Staff can quickly become overburdened as they attempt to resolve discrepancies, respond to member complaints, or meet regulatory inquiries.
Accurate provider information helps eliminate these setbacks, allowing your teams to focus on high-value projects and deliver meaningful results. By enhancing your workflows, you minimize wasted effort and help your organization operate at peak efficiency.
How Do You Validate Provider Data?
- Use a centralized platform like Quest Enterprise Services® (QES®) Accuracy
- Automate outreach to providers for quarterly attestations
- Monitor data freshness and flag outdated or inconsistent records
- Integrate external data sources for enhanced verification (for example, licensing boards, hospital affiliations, etc.)
- Implement standardized data entry practices.
Making Provider Data Accuracy a Priority
Provider data validation isn’t optional—the stakes are simply too high. Whether you’re aiming to meet compliance standards, improve the member experience, or enhance operational efficiency, accurate data has the power to transform how your organization works.
By making provider data validation a priority, you build a strong foundation for a more efficient, member-focused, and compliant health plan. And with the right processes in place, you’ll spend less time fixing errors and more time achieving meaningful outcomes that benefit both your members and your organization.
Elevate Your Provider Data Accuracy
Discover how Quest Enterprise Services® (QES®) Accuracy can make a difference. Our comprehensive solutions enhance your process, offer better data transparency, reduce ghost networks, and improve compliance. Empower your organization to excel in the evolving healthcare landscape. Learn more about Quest Enterprise Services® (QES®) Accuracy today!
Proven Solutions for Your Provider Network Management
Looking to simplify your workload? Let Quest Analytics take on the heavy lifting! Our solutions and dedicated team specialize in provider data accuracy and provider network adequacy for various lines of businesses, including Medicare Advantage, Medicaid and Commercial. Schedule a strategy session today and see how we can help you every step of the way.