“Hands down, the most frequently asked question we get here at Quest Analytics is: ‘How can we be more strategic when it comes to network development?’” notes Eliza Hoffman, VP of Regional Payers at Quest Analytics®. It’s a great question—and for healthcare payers, tackling it is foundational to thriving in today’s dynamic healthcare environment.
Building a Compliant & Marketable Provider Network with Quest Analytics
How can you be more strategic with network development? Eliza Hoffman, VP of Regional Payers, shares expert tips on leveraging provider data, clinical activity, and performance metrics to build smarter networks. Watch now for actionable insights powered by Quest Enterprise Services!
A recent survey of healthcare payer executives by Quest Analytics and Becker’s Healthcare revealed that top strategic priorities include increasing member satisfaction, improving clinical quality, and driving membership growth in existing markets. By leveraging comprehensive and reliable data insights, you can build a high-quality, marketable healthcare provider network that supports each of these critical objectives.
Enhance Member Satisfaction
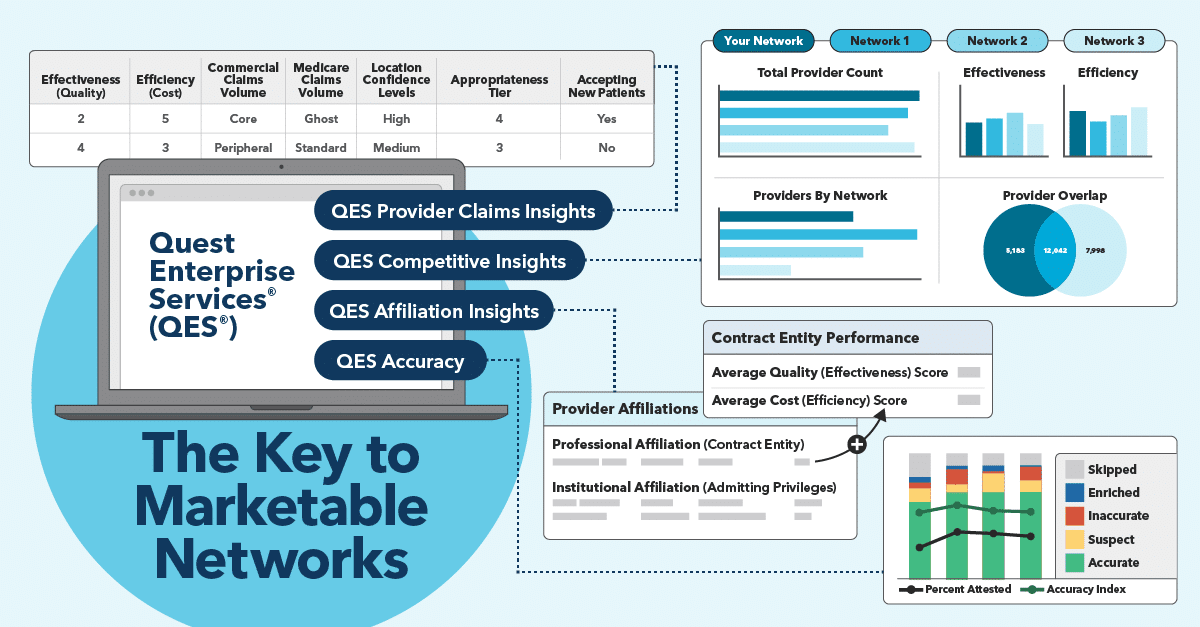
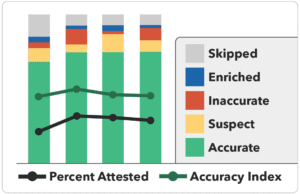
Satisfied members are more likely to stay loyal to your health plan, helping to reduce costly churn and continue personal referral marketing. Improving member satisfaction starts with provider data accuracy. Outdated or incorrect provider information, like wrong phone numbers or listings for inactive providers, can frustrate members and create unnecessary barriers to care. With the Quest Enterprise Services® (QES®) Accuracy, you can elevate provider data integrity and the membership experience at the same time.
Network design also plays a role in membership satisfaction. A marketable network offers convenient, reputable provider options without long wait times. QES Provider Claims Insights can help you optimize your network and address network gaps to better meet your members’ needs, while QES Affiliation Insights can help ensure in-network alignment and reduce surprise billing risk for your members.
Deliver Better care at Lower Cost
A strategic approach to provider contracting will help your network deliver high-quality, cost-effective care. Partnering with providers and health systems with proven track records will make your network even more appealing to prospective members, and comprehensive specialty coverage can lead to more coordinated care and lower out-of-network costs.
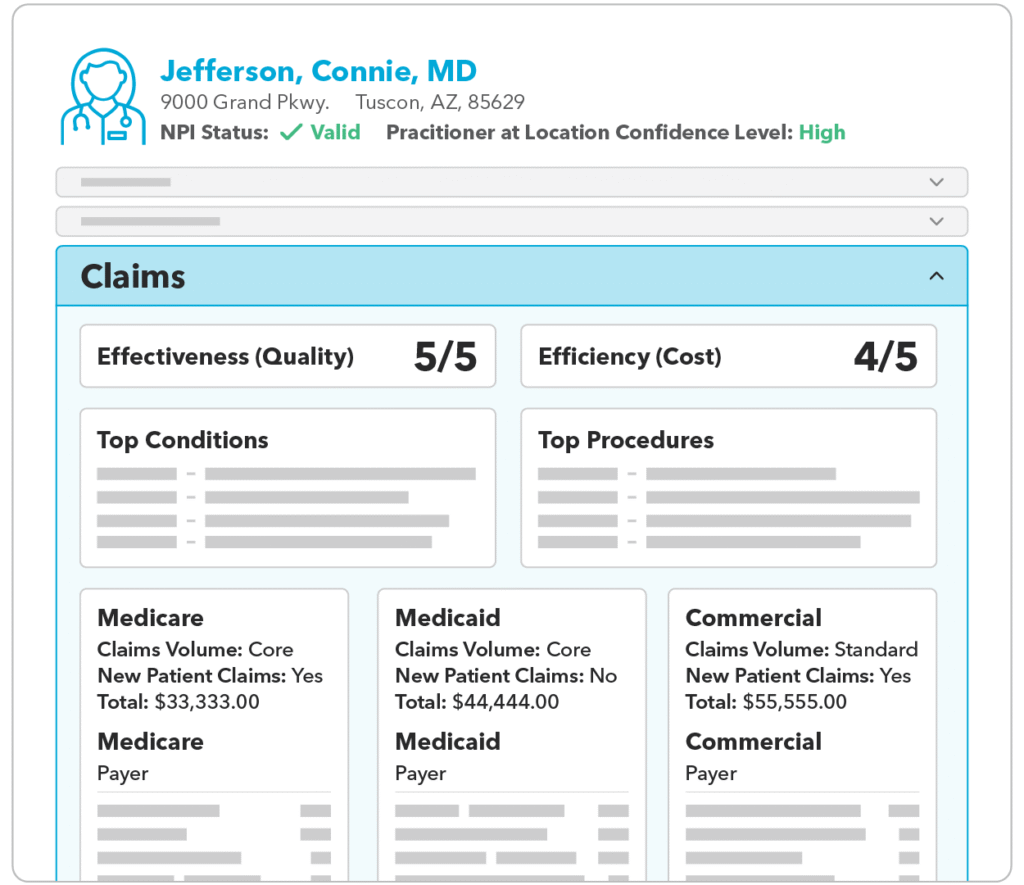
If you’re debating about which providers will help you improve clinical quality, QES Provider Claims Insights can help. Our proprietary, comprehensive database includes more than 5 billion annual medical and pharmaceutical claims, plus additional provider performance metrics through Quest Analytics’ partnership with Arcadia’s CareJourney and Motive Practicing Wisely. Drawing on this wealth of data, you can quickly analyze providers’ clinical activity, top conditions and procedures, and efficiency and effectiveness scores, giving you a much deeper understanding of which providers will add the most value to your network. You can also assess the cost, quality, and payer mix, helping you determine which providers to prioritize for contracting.
Strengthen Your Position in New and Existing Markets
To make your network attractive to new employers and members, you’ll want to understand your competitive position. QES Competitive Insights provides valuable intelligence on the other players in your target market, showing you how your network compares and where you can optimize to meet market needs. For example, if your network’s specialists are concentrated downtown in a particular metropolitan area, you might want to contract with providers in the suburbs to attract more suburban members. Competitive Insights can also help you assess whether it’s worth expanding into a new market or line of business before you commit.
“Compliance keeps you in the game,” said Bob Tavernier, Sales Solutions Executive at Quest Analytics, “but to compete and thrive, you need to exceed the baseline.”
If you’re ready to use data-driven intelligence to increase the marketability of your healthcare provider network, Quest Analytics can help. Schedule a complimentary consultation with one of our experts today to learn more.
Related Network Performance Resources
Know Your Data, Grow Your Business
Get a complimentary strategy session with a Quest Analytics expert to learn how we can help you maintain network adequacy, improve data accuracy and achieve astonishing efficiencies.