Quest Enterprise Services™ (QES™)
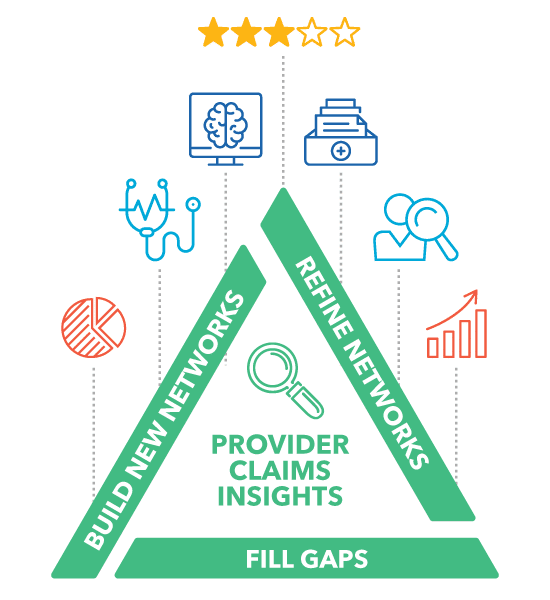
Provider Claims Insights
Build and Optimize Networks with Actionable Provider Insights
Discover how Provider Claims Insights (PCI) empowers healthcare network strategists to enhance care quality and cost-efficiency through provider data and analytics.

QES Provider Claims Insights
Your solution for powerful provider performance analytics
Unlock the full potential of your healthcare networks with Provider Claims Insights (PCI). Leveraging a robust claims database, including the full spectrum of payers and lines of business, PCI brings powerful provider performance analytics into the Quest Enterprise Services™ (QES™) platform. QES PCI substantially enhances provider network optimization, ensuring that every network decision is informed, every action is strategic, and every outcome is optimized for the highest standard of care.
Provider Network Optimization
Fill network gaps efficiently with high-quality, low-cost providers that are proven to be active in the line of business you care about.
Comprehensive Data
Access our premier proprietary claims database encompassing over 5 billion yearly claims across Medicare, Medicaid, and commercial lines. Enhance your QES with this wealth of data, outpacing internal and external sources.
Regulatory Compliance
Meet regulatory requirements by providing insights into a provider’s level of clinical activity, which is crucial for member satisfaction and retention and helps avoid penalties from audits testing provider directory accuracy.
Revenue Optimization
Use cost and quality metrics to build and refine provider networks for cost-effective care that helps reduce medical expenses and improve profitability.
- Popular Features
- Use Cases
- Related Solutions
- Related Resources
Popular Features
Discover PCI’s top features – your toolkit to help you better understand provider performance so that you can build, expand, and optimize your networks strategically.
Provider Claims Data Insights
Provides unparalleled insights into provider performance and network management leveraging our comprehensive provider claims database.
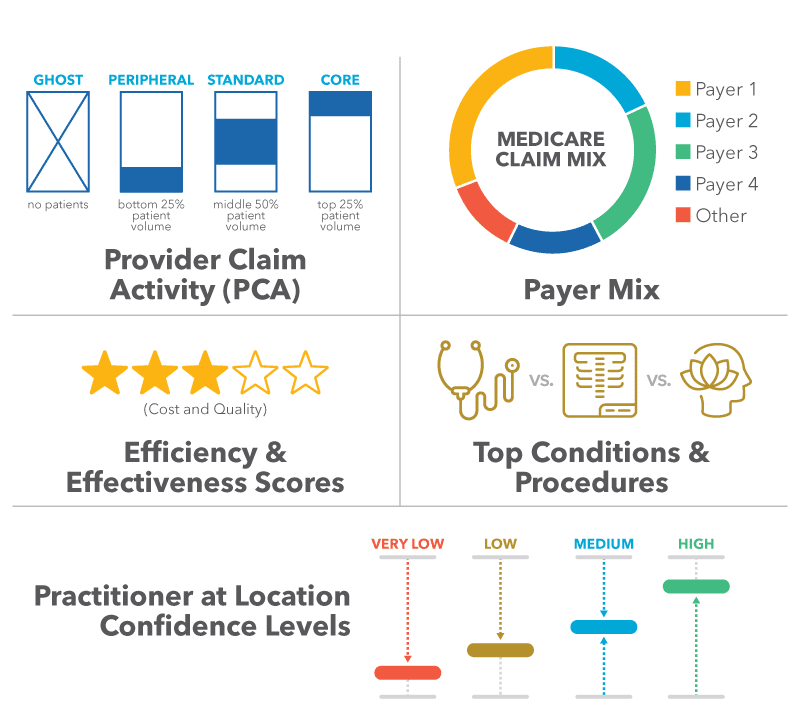
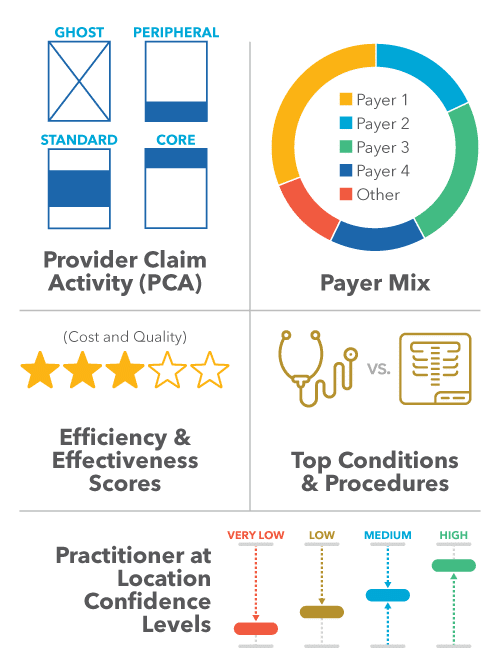
Provider Clinical Activity
Ensure regulatory compliance and prevent penalties by identifying inactive, or ghost, providers through provider clinical activity data.
Executive Dashboard
Access intuitive dashboards for monitoring network performance across key measures, enhancing decision-making capabilities.
Efficiency and Effectiveness Scores
Review and measure providers based on efficiency and effectiveness, aiding in the prioritization during the network gap-filling process.
Top Procedures and Conditions
Leverage valuable claims-based metrics, including top procedures and conditions, for a targeted approach in network gap management.
Practitioner At Location Confidence
Ensure accurate provider recruitment and gap-filling with additional insights within PCI for practitioners at the location.
Provider Claims Insights in Action
Explore how PCI can revolutionize your provider network management strategy, deliver measurable results, and drive success for healthcare networks nationwide.
More Efficient Gap Filling
Accelerate the closure of network gaps with actively practicing specialists, ensuring members can access the care they need.
Network Refinement
Streamline your network for peak performance, enhancing efficiency and member experiences with strategic provider alignment.
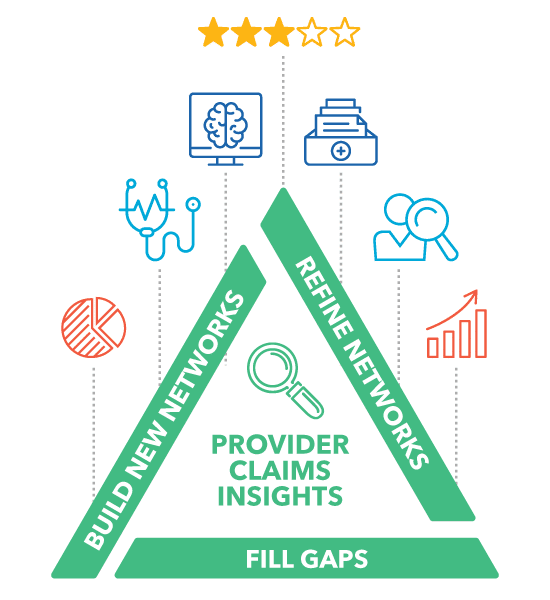
New Network Builds or Expansion
Expand your network rapidly to meet strategic goals, ensuring comprehensive coverage and member satisfaction.
Member Steerage and Referral Decision Support
Direct members to high-value care, optimizing healthcare outcomes and cost-efficiency with informed provider referrals.
Related Solutions
Through Quest Enterprise Services™ (QES™), you have access to an enterprise platform that enables you to enhance your network’s performance with a comprehensive suite of solutions tailored to complement QES PCI. These solutions are synergistically designed to work in concert, providing you with the tools you need to construct networks that are compliant, competitive, accurate, and high performing.
Combine QES PCI with QES Adequacy to achieve effortless measurement, management, monitoring, and modeling of your network adequacy, supporting compliance while helping ensure your members can access the right providers for their unique needs.
Pair QES PCI with QES Accuracy to maintain you have the most accurate directory of providers, ensuring that your members have access to the proper care when needed.
Compare your network to your competitors with Network Benchmarking and leverage the information from QES PCI to compare provider cost, quality and clinical activity to your peers.
Measure your health system’s impact on payer network adequacy. Viewing your provider footprint from a payer perspective can be a valuable tool for payer negotiations or evaluating expansion opportunities.
Create the optimal network by recruiting the right providers in terms of access, provider performance, competitive overlap, and other KPIs.
With Quest Enterprise Services, we enable you to bring in other relevant data sources like Motive Practicing Wisely to enhance your health plan data analysis.
Discover More
Dive into additional resources for more information and valuable insights.
GET STARTED WITH PROVIDER CLAIMS INSIGHTS
Quest Enterprise Services Provider Claims Insights helps you improve the value of your provider network by ensuring it is adequate, accurate and active! Schedule a complimentary strategy session today to learn more.

Start a Conversation Today!