Quest Enterprise Services® (QES®)
Navigate Provider and Facility Connections with Greater Clarity
QES® Affiliation Insights helps you understand how providers are organized by practice, group, and care sites, allowing you to identify the right contracting entities and design smarter healthcare provider networks based on affiliations and care delivery patterns.

QES® Affiliation Insights
Optimize healthcare provider network management and design with QES® Affiliation Insights, which brings clarity to your provider network by revealing the complex relationships between healthcare providers, organizations, and facilities that shape network contracting and care delivery.
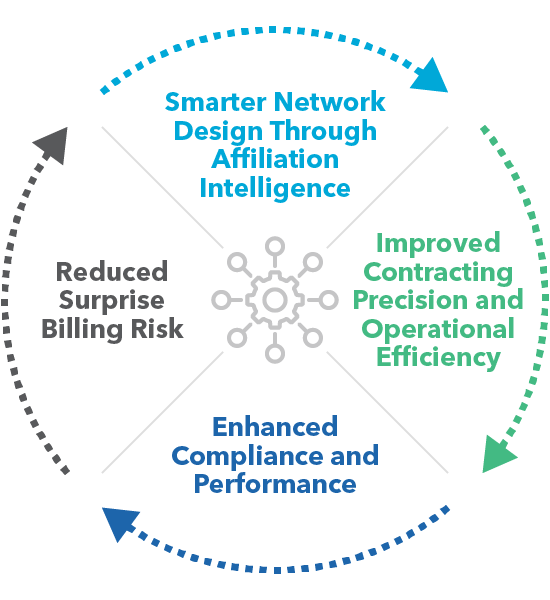
Integrated directly into QES®, Affiliation Insights allows you to view the organizations where individual providers are contracted and provides visibility into the facilities where providers treat patients. By combining this information, you can better understand how to contract with providers and determine which facilities should be included in your network based on provider practice patterns. Affiliation Insights supports you at every stage of the Healthcare Provider Network Lifecycle, leading to smarter, more effective network design, network optimization, and network management.
Design Smarter Provider Networks
Build smarter networks by understanding how providers and facilities align through professional and institutional affiliations. Make confident inclusion decisions that identify high-impact entities that drive strategic network growth.
Enhance Compliance and Network Performance
Visualize the impact of provider groups and contract entities on closing network adequacy gaps. Gain insights into provider mix, quality, and cost at the entity level by integrating Provider Claims Insights.
Improve Contracting and Operational Efficiencies
Identify the most likely contracting authority and align providers under the right entities. Streamline negotiations and improve operational efficiency with targeted, data-driven decisions.
Reduce Surprise Billing Risk
Help ensure in-network alignment between providers and facilities to minimize out-of-network charges and improve the member experience.
- Popular Features
- Use Cases
- Related Solutions
- Related Resources
Popular Features
Contract Entity Intelligence
Provider-Facility Alignment
High-Impact Entity Finder
Entity-Level Performance View
With the addition of Provider Claims Insights, access provider cost and quality data at the contract entity level to evaluate performance and make more informed inclusions and contracting decisions.
Network Impact Modeling
Contract Entity Profiles
QES® Affiliation Insights in Action
QES Affiliation Insights transforms how you design and manage networks by revealing the true structure behind provider and facility relationships. From accelerating network adequacy modeling to streamlining contracting and scaling into new markets, it equips teams with the intelligence needed to build smarter, more compliant networks faster.
Accelerate Network Modeling with Entity-Level Precision
Shift from provider-level network modeling to contract entity-level modeling. By understanding how providers contract, you can drastically reduce network analysis time, close network gaps more efficiently, and avoid unnecessary overbuilding.
Improve Network Integrity with Hidden Structure Visibility
Uncover hidden affiliations between providers and facilities that were not visible in traditional data sources. This helps compliance teams proactively address network adequacy risks, improve audit readiness, and support more accurate decisions regarding provider inclusion.
Streamline Contracting with Verified Provider-Facility Alignment
Identify the most likely contracting authority across a fragmented provider landscape. This clarity can enable you to consolidate outreach, reduce negotiation cycles, and improve operational efficiency across all lines of business.
Scale Network Design for New Market Entry
Quickly identify high-impact contract entities and prioritize them for inclusion when entering a new state. This approach allows you to build a compliant, high-performing network faster, while aligning with strategic growth goals.
Related Solutions
Through Quest Enterprise Services® (QES®), you have access to an enterprise platform that enables you to enhance network performance with a comprehensive suite of solutions tailored to complement QES Affiliation Insights. These solutions are synergistically designed to work in concert, providing you with the tools you need to construct networks that are compliant, competitive, accurate, and high performing.
QES Adequacy
QES Affiliation Insights is seamlessly integrated into QES Adequacy, helping you efficiently measure, manage, monitor, and model your network within the platform you are already using.
Learn MoreQES Provider Claims Insights
Leverage QES Affiliation Insights in combination with QES PCI data to gain a thorough understanding of your network. By assessing provider costs, quality, and clinical activity, you can pinpoint areas for improvement, make informed strategic decisions, and ultimately enhance the performance of your provider network and member satisfaction.
Learn MoreQES Scenario Modeling
Create and develop scenarios to help you plan and predict how different provider additions or terminations across networks might impact your network.
QES Accuracy
Pair QES Affiliation Insights with QES Accuracy to maintain the most accurate directory of providers, ensuring that your members have access to the proper care when needed.
Learn More
Discover More
Dive into additional resources for more information and valuable insights.
Get Started with QES Affiliation Insights
Discover smarter solutions for contracting and network design. Schedule a complimentary consultation to explore how we can help you achieve your goals.
Schedule a complimentary consultation with one of our network experts today to learn more.

Start a Conversation Today!









