FIVE PROVIDER DATA MANAGEMENT TIPS FOR HEALTH PLANS
Provider networks change faster than you can say, “I’m calling to make an appointment.” Okay, maybe not that fast, but a typical provider network can change up to 20% in a year. When you combine the annual percentage of change, with the increase in provider data accuracy and transparency requirements, it adds up quickly. To keep up with all the ongoing new demands, provider network management teams are reevaluating their data management strategies and processes.
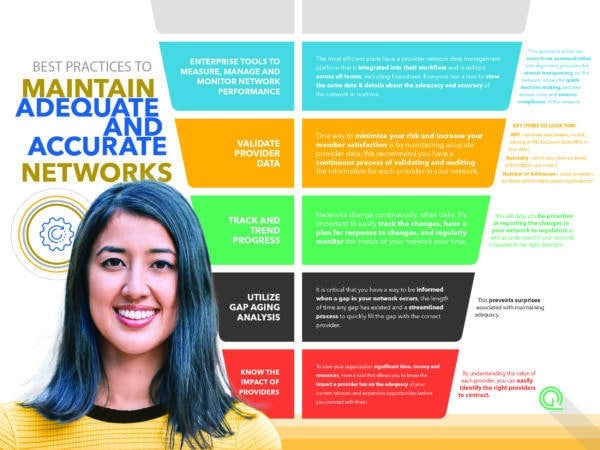
If you’re building a new network or maintaining a current network, it can be tough to know where to begin. Here are five fundamentals your team can use to maintain accurate and adequate provider networks. Download Now
HOW PROVIDER NETWORK MANAGEMENT TEAMS POSITION THEMSELVES FOR SUCCESS
CMS Resource Hub
Looking for more tips to help you stay review-ready and compliant-confident with CMS? We’ve got them! Explore our CMS Resource Hub to find our growing collection of guides, videos and tools to help you achieve your compliance and service area expansion goals.