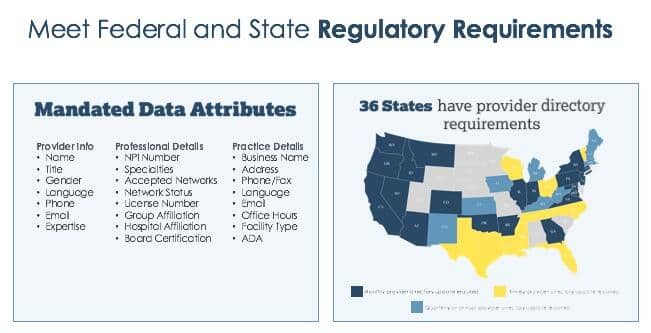
When we say the strictest provider compliance law in the country, we’re not kidding. Although other state and federal regulators, the Centers for Medicare & Medicaid Services (CMS) for example, are starting to incorporate rules around provider directory data, SB-137 requires health plans to reach out to all contracted providers on a quarterly basis to update over 100 data attributes including:
- Provider Name
- NPI
- Specialty
- Admitting privileges at facilities
- Panel status
Health plans must also update their online provider directory data at least weekly when informed of any changes from providers.
Several questions are probably running through your mind, such as:
How do I ensure my internal and external processes are 100% SB-137 compliant? What steps can I take to achieve better data accuracy within my health plan organization? How can I achieve better data, better networks, and a better consumer experience? How do I select the right vendor(s) to help?
The answer to that last question, choosing the right vendor to help, is the most critical. The right vendor can help guide you through all the answers. That’s why we’ve gathered seven best practices for choosing the right vendor for you.
- Ensure that the vendor collects data through primary source data attestations and helps you be audit ready
- Make sure your vendor is doing quarterly outreach to 100% of your provider network
- Build effective multimodal outreach methods that are user-friendly for providers
- Verify that your vendor is SB-137 compliant and approved by the DMHC
- Check that your provider rosters are not causing conflicting data errors
- Choose a vendor that helps you understand how accuracy changes impact your network adequacy
- The vendor helps you improve your provider directory consumer experience
Ensure that the vendor collects data through primary source data attestations and helps you be audit ready
There is no safe harbor without having data about all communications with providers accessible. As you create internal processes to manage your provider directory accuracy, tracking changes and when they’re made is crucial. This metadata can help you resolve conflicting updates, or help you deal with any potential audits by a regulatory agency like the Department of Managed Health Care (CA DMHC) or CMS.
When choosing your vendor, ask how they manage metadata, and how it can help you address conflicting changes and potential audits. Some vendors will prepare you for any potential audits that may come your way. At Quest Analytics, we provide full transparency to support our health plan clients, through any auditing procedures.
Make sure vendor is doing quarterly outreach to 100% of your provider network
SB-137 requires you to update information with providers at least quarterly. Additionally, if there are any provider changes, health plans must update their online provider directories accordingly on a weekly basis.
Build effective multimodal outreach methods that are user-friendly for providers
When you’re working with vendors, ask how they reach out to providers. What kind of relationship do they have with providers? How often do they reach out to them? In what form do they communicate with them. Is it via email, fax, phone, mail, or all of the above? Ideally, you want diverse and consistent outreach methods that will collect the most accurate data online.
Verify that your vendor is SB-137 compliant and approved by the DMHC
It’s important to verify that the vendor you’re working with is SB-137 compliant. You can contact your state regulator at the Department of Managed Health Care to learn which vendors are SB-137 compliant. There are multiple vendors out there that can help you comply with SB-137, including the Quest Analytics’ Accuracy Solution — BetterDoctor.
You’ll also want to understand the SB-137 requirements. Under this state provider directory law, health plans must:
- utilize uniform data definitions (defined by CMS, California Dept. of Insurance (CDI), & DMHC),
- update online provider directories at least quarterly,
- update online provider directory data weekly when informed of a change, and
- ensure that directories have all relevant attributes including provider name, NPI, admitting privileges, and accepting new patients.
And that’s just for SB-137. To help create efficiencies for you and your organization, you’ll want to work with a vendor that can help you maintain compliance with other state and federal regulations, such as network adequacy and provider directory requirements for Medicare Advantage.
Check that your provider rosters are not causing conflicting data errors
Managing provider data is very complex. When the Quest Analytics’ Accuracy Solution — BetterDoctor— performs outreach directly to providers’ offices, our goal is to make practitioners and their office staff the primary owners of their data. That’s because they know it best. We have lived too long in an age where stale data is the norm. The process of collecting provider data through a health plan or IPA and having to wait for those updates to be acknowledged, processed and visible is antiquated and ineffective. When choosing a vendor ask about their outreach process. You’ll want to hear that they collect primary source attestations.
When the CMS performs ‘secret shopper’ audits, they directly contact healthcare provider offices. CMS considers individuals answering phone calls from members as the source of truth for provider data. It is in your best interest to make sure provider group rosters are not causing conflicting data errors in your provider directories.
For example, Quest Analytics performs two-factor authentication to validate provider status changes (e.g., deceased, retired, not at location) received through a pre-populated online form. We share these updates with the medical group(s) for roster integration, and with a health plan(s) to maintain directory accuracy, along with other critical errors identified (e.g., missing appointment phone number, incomplete address). Medical groups may independently partner with Quest Analytics for a group roster accuracy assessment and maintenance to meet SB-137 compliance and to more easily submit this data to health plans and other regulatory entities.
Choose a vendor that helps you understand how accuracy changes impact your network adequacy
As you clean up your data, this may impact your network adequacy results. Ask your vendor if they can help you condense your workflows to improve how you process changes quickly and efficiently. Additionally, make sure the vendor you work with offers simple data integration and ensures that you can get changes live in your directory in a timely manner.
At Quest Analytics, we understand how data accuracy and network adequacy are inextricably linked. Our Accuracy Solution integrates directly with the Quest Cloud Solution™ allowing you to monitor and trend changes within your network. As you incorporate accuracy changes, our cloud solution helps you identify any emerging gaps in adequacy and the providers available to fill them.
The vendor helps you improve your provider directory consumer experience
With Quest Analytics, we work with our health plans to encourage ongoing provider participation and consumer selection by educating the consumer with the results of the attested data. This approach has a direct impact on the consumer experience as well as provides additional incentives for the providers to continue ongoing participation.
Would you like to learn more about how to become SB-137 compliant? Let’s talk. Email laura.pereyra@questanalytics.com, and she’ll connect you with the best person to answer your specific questions.
At Quest Analytics we want to help health plans achieve Better Data. Better Networks. Better Experience. Quest Analytics is the provider data management and network analytics services company the nation’s health plans trust to provide a better experience for plan members by ensuring their networks comply with access, adequacy, and accuracy standards.