Provider data management is complex. We all know that. What we do not always do is go into deeper exploration to learn where exactly that complexity comes from. BetterDoctor provider portal helps thousands of doctors, office managers and administrators on a daily basis to update their provider directory information. Here is what we learned about the intricacies of managing this data to maintain its highest quality.
WHAT DOES THE WORKWEEK OF AN AVERAGE DOCTOR ACTUALLY LOOK LIKE?
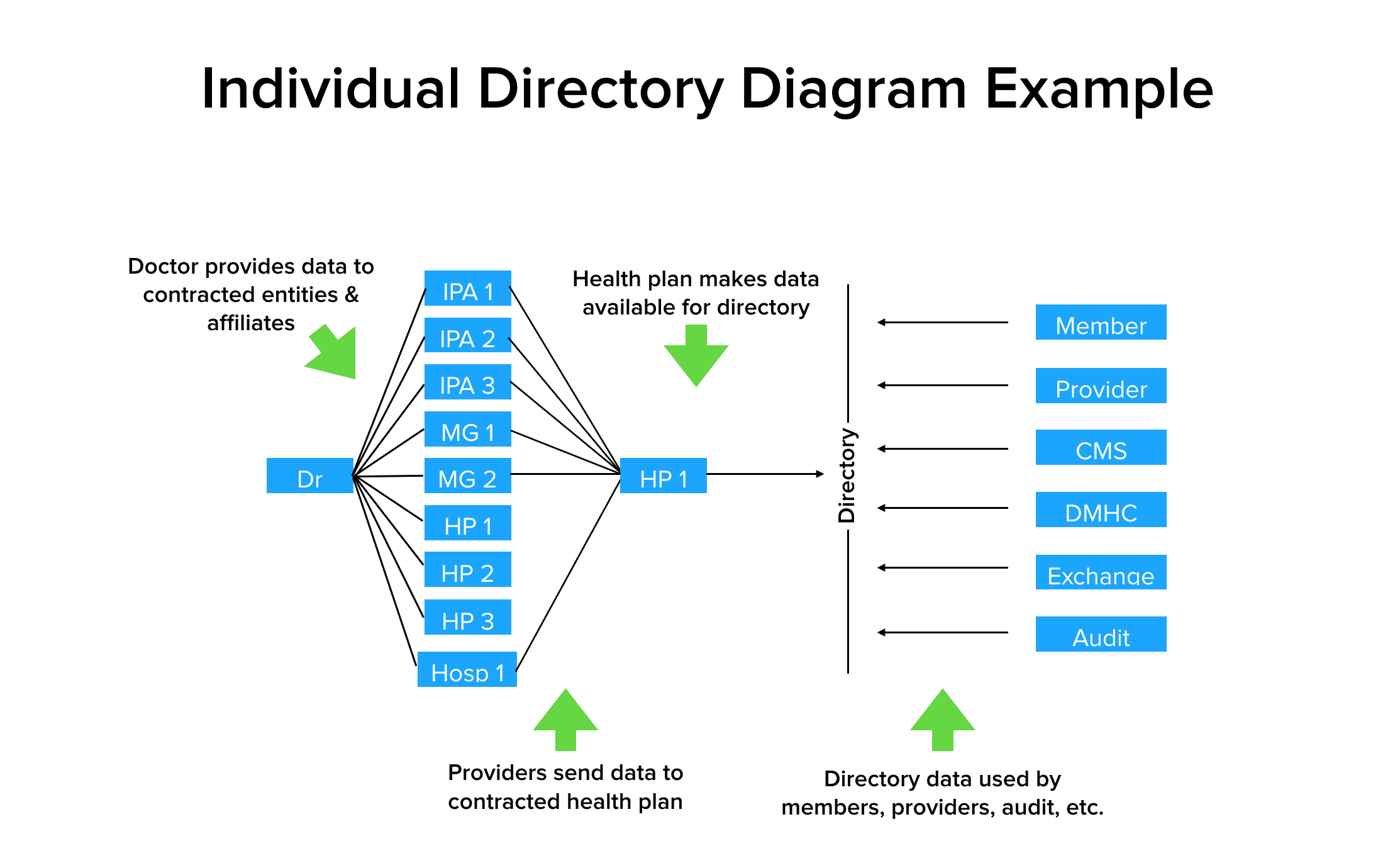
As an example, let’s picture the workweek of Dr. M. He works at a medical group that contracts with 5 health plans Monday through Tuesday. He then works at a private practice contracted with 3 health care plans and 4 IPAs Wednesday through Thursday. Then he works at a hospital contracted with 12 health care plans and 10 IPAs on Fridays. Pretty straightforward, right?
Not so much. Dr. M theoretically is responsible for regularly reporting his demographic data to all his directly contracted entities which then populate his data into their provider directories. In our example that data would go to 3 IPAs, 2 medical groups, 3 health plans, and one hospital. All this data ultimately ends up in a health plan provider directory which members, other providers, regulatory entities — from CMS to local regulatory bodies and state exchanges — can see and access. The same provider data is often also used to audit whether a health plan has a network that gives consumers adequate access coverage.
WHERE DOES THE WEB OF DATA GET MORE COMPLEX?
So let’s get deeper into how managing this web of data gets a little more complex. Below is an example data challenge. It illustrates how the different entities that Dr. M works with recognize different certifications. They even look at his primary and secondary specialty differently, depending on what his certifications deem acceptable. You can imagine how data in a provider directory may get a doctor’s specialty wrong. Different entities view Dr. M’s certifications differently.
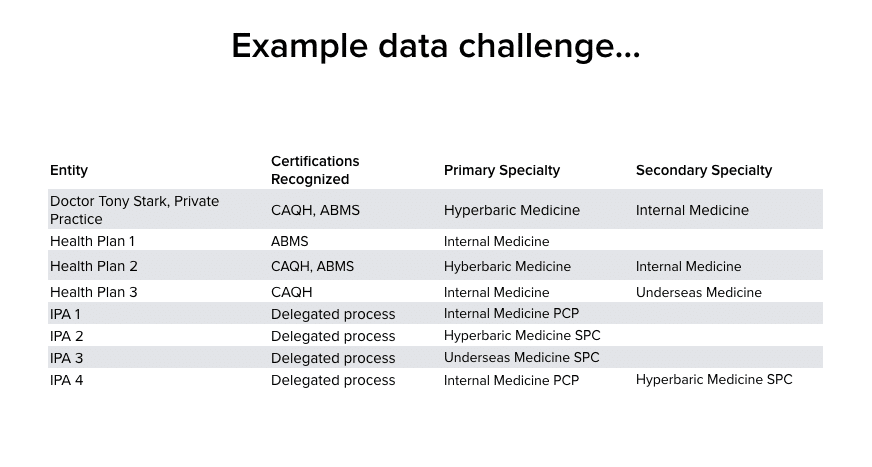
This example data challenge shows the complexity in how certifications and specialities may be aggregated and/or recognized differently by the contract relationships providers hold.
WHAT HAPPENS WHEN A DOCTOR RECEIVES REQUEST TO UPDATE THEIR DATA?
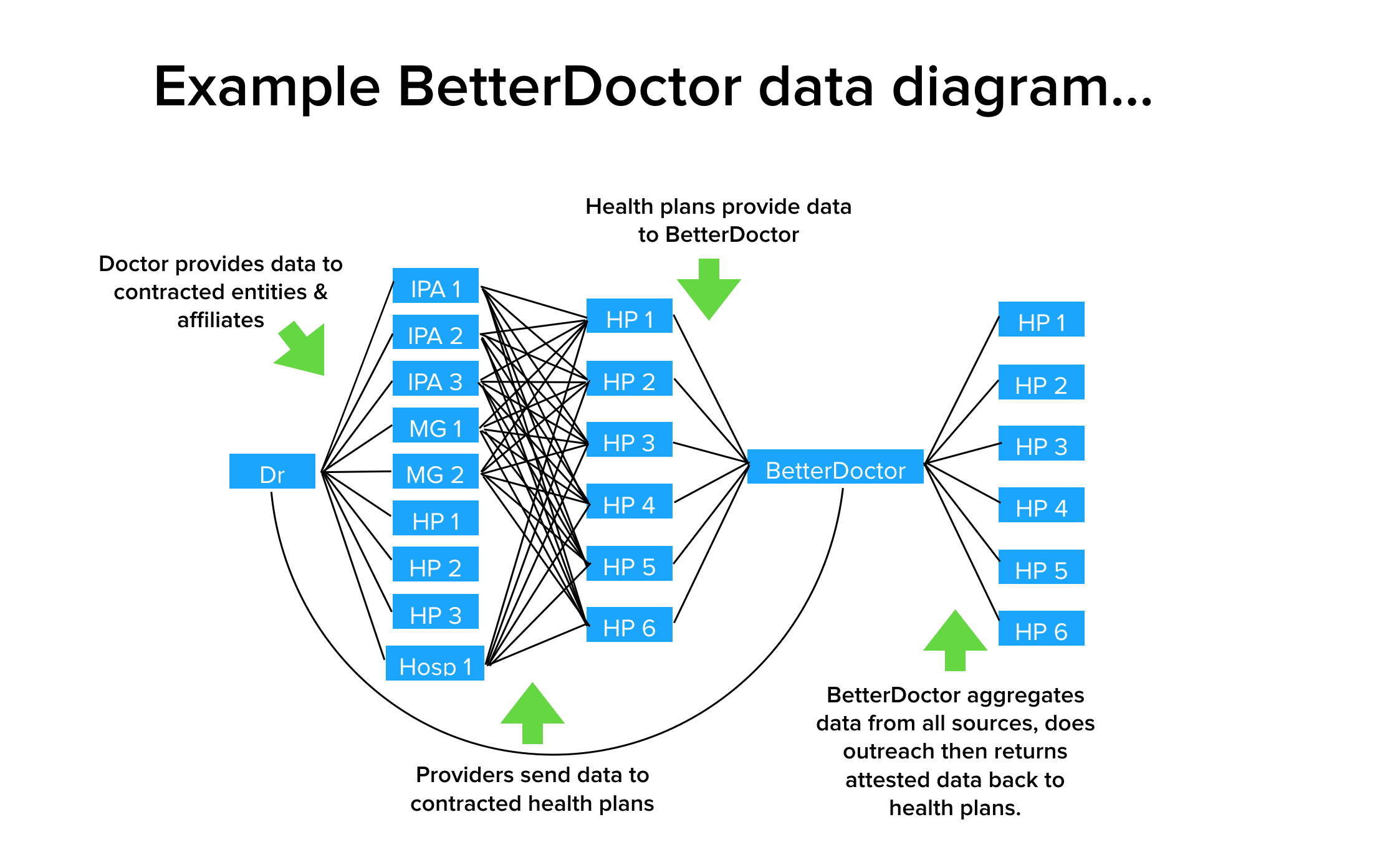
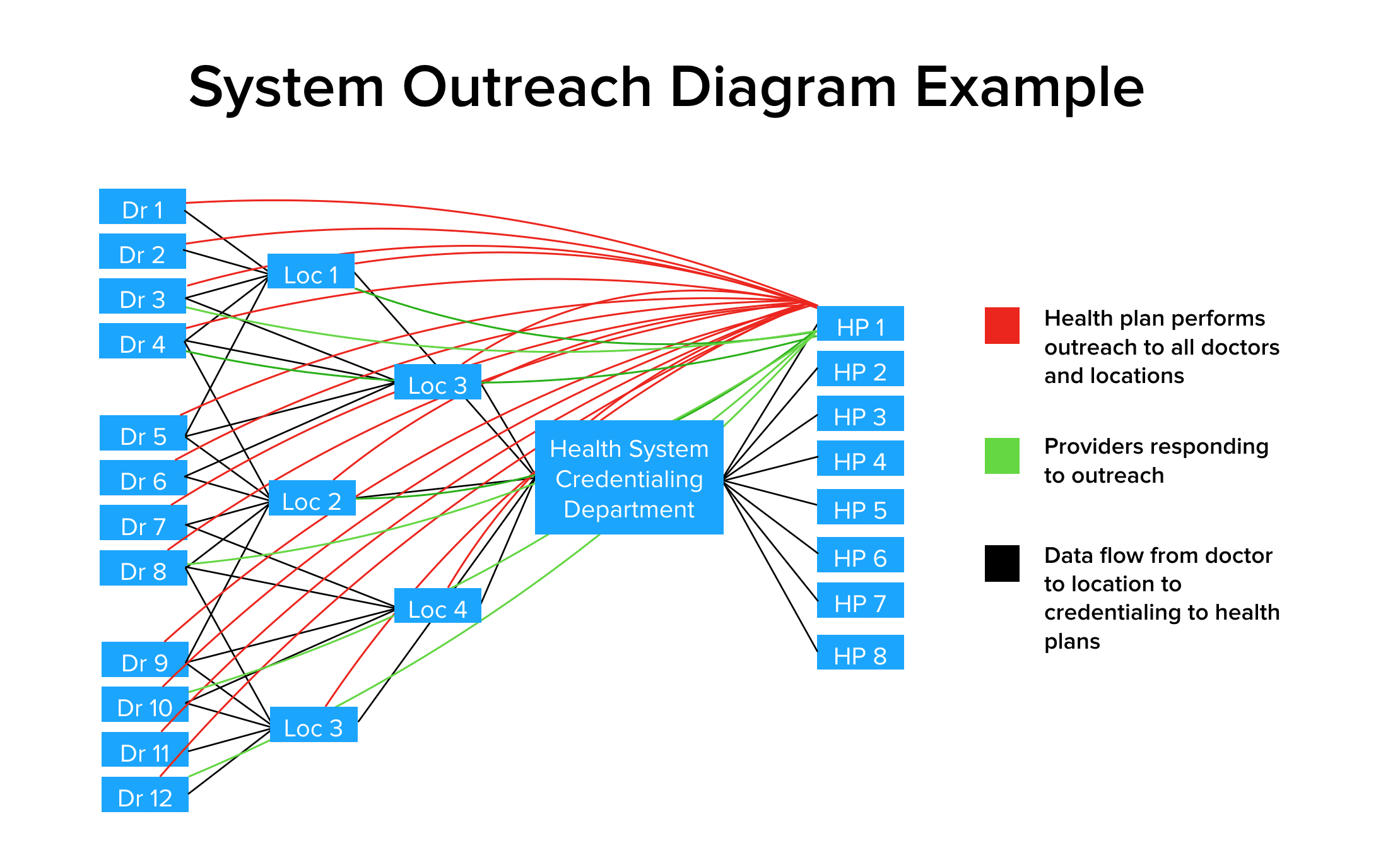
So now, let’s attempt to understand what happens when an entity working on behalf of a health plan, like say BetterDoctor, reaches out to Dr. M.
The below data diagram shows Dr. M updating his data with BetterDoctor. We aggregate data from all sources, do outreach, then return the attested data back to health plans. Where things may get messy is when Dr. M provides his data to the 3 IPAs, 2 medical groups, 3 health plans, and 1 hospital. All these entities attempt to update their data with all the health plans they work with but a lot can get lost in translation. BetterDoctor steps in by taking the data from all sources — the provider themselves, the health group, and the health plan. We attempt to identify what appears to be the most correct representation of the data, then we work to clarify what is the true representation of the data by verifying it straight from the source.
HOW CAN WE MOVE TOWARD HIGHER QUALITY PROVIDER DIRECTORY DATA?
When BetterDoctor does outreach directly to the providers, our goal is to make the providers the primary owners of their own data because they know it best. They can update their data directly without having to go through a health care plan or IPA; then waiting for those updates to be acknowledged, processed and visible. We have lived too long in an age where stale data is the norm.
When the Centers for Medicare & Medicaid Services (CMS) perform their ‘secret shopper’ audit studies, they directly contact the doctor’s office. At the end of the day, CMS audits consider the providers as the only entities that know which data is correct.
BetterDoctor helps health plans cut through all the complexity in collecting the data that matters when ensuring that provider directory meets data accuracy and regulatory compliance requirements.