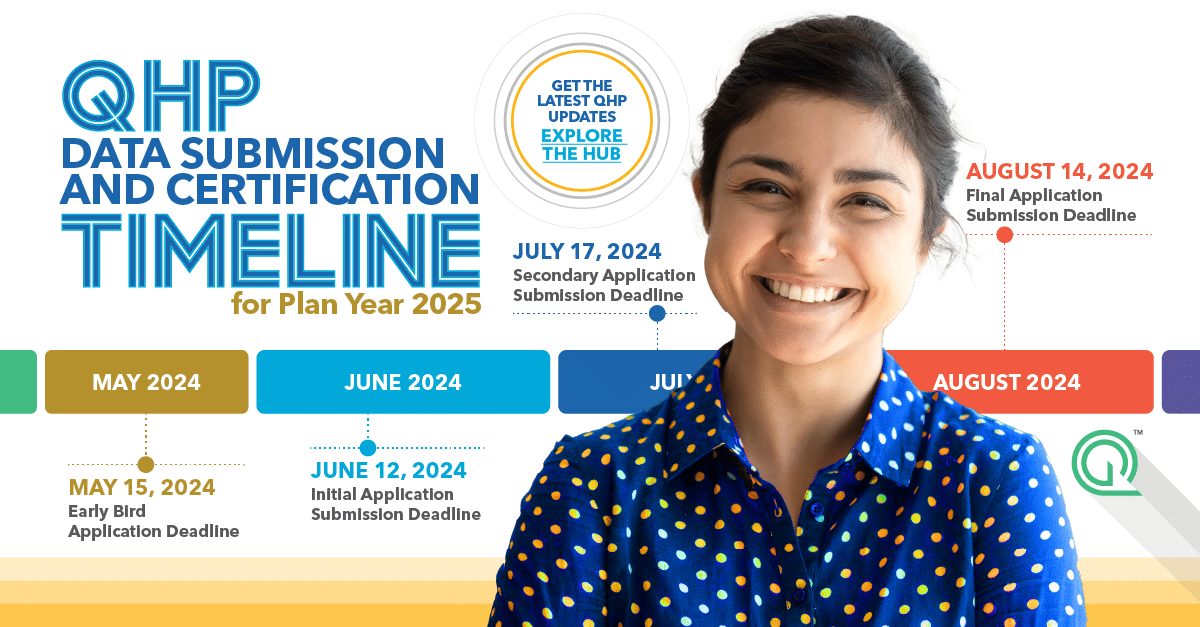
Who doesn’t love a good calendar? We know we do. Whether you’re deep into network adequacy updates or juggling deadlines left and right, we’ve got your back. Our handy calendar lays out the crucial submission dates for Qualified Health Plan (QHP) issuers on Federally-facilitated Exchanges. As a bonus, we’ll keep it updated for you! Go ahead and download it, bookmark it, print it – and share it with a colleague.
Key QHP Network Adequacy Application Deadlines PY2025
Get a sneak peek at important dates! Check out the key dates below for an overview of application deadlines. For more details and additional dates, grab the calendar today!
Early Bird Application Deadline
May 15, 2024
Optional Early Bird deadline for Issuers to submit QHP Applications to CMS.
Initial Application Submission Deadline
June 12, 2024
The initial deadline for Issuers to submit QHP Applications to CMS, including Machine-Readable Index URLs and Plan ID Crosswalk data.
Secondary Application Submission Deadline
July 17, 2024
Deadline for Issuers to submit their QHP Application Rates Table Templates to CMS.
Optional deadline for Issuers to submit corrected QHP Application data to CMS.
Final Application Deadline
August 14, 2024
Deadline for Issuers to submit changes to their QHP Applications and to submit marketing URL data.
Data Tips for Network Adequacy Data Submission PY2025
Need extra help with your data submissions? We’ve got you covered there too! Download our exclusive 6 tips for a successful Network Adequacy Data Submission. With important changes and data requirements in the Network Adequacy template, these tips will be your lifesaver. Don’t miss out on vital information – download now and ace your submissions!
Stay ahead with the latest QHP network adequacy requirements! Download our policy brief now to discover the key changes and updates that will shape the future of QHP certification. Don’t miss out on essential insights for your plans!
Download the Policy Brief
More QHP Certification and Network Adequacy Resources
Proven Solutions for Your Provider Network Management
Gain provider data integrity and drive maximum impact from your provider network with Quest Analytics CCIIO QHP Network Adequacy Template. Our experts will help you create, manage, and monitor your provider network quickly and easily. Schedule your strategy session now!