Las Vegas, NV, June 17, 2025 — Quest Analytics, the leader in provider network design and management solutions, announces the launch of QES Affiliation Insights, a new capability within its Quest Enterprise Services® (QES) Performance Suite of Solutions. This innovation gives health plans and healthcare organizations a clear view into the complex web of provider affiliations and contracting entities — empowering them to make smarter, faster decisions for network design, provider contracting, and network performance optimization.
QES Affiliation Insights allows users to view the organizations with which individual providers are contracted. It also offers visibility into the facilities where providers treat patients, such as hospitals and Ambulatory Surgery Centers (ASCs). By combining this information, health plans can better understand how to contract with providers and determine which facilities should be included in their network based on provider practice patterns.
“With QES Affiliation Insights, health plans operate from a high-fidelity database that connects contracting, care management, and performance strategy,” said Steve Levin, CEO of Quest Analytics. “By understanding how providers are affiliated both clinically and for contracting, executives can improve Medical Loss Ratio (MLR), reduce inefficiencies, and make confident decisions that align with both business goals and member needs. Given recent trends in health system consolidation, these insights couldn’t be timelier.”
Quest Analytics to Spotlight Performance Intelligence at AHIP 2025
Innovation Spotlight Session: Insights to Transform Provider Network Strategy for Improved Performance
Quest Analytics® introduces QES® Affiliation Insights to help health plans and insurers enhance their approach to provider network strategies. Presented during AHIP 2025, this session by Brent Sanders, Chief Commercial Officer at Quest Analytics, highlights the importance of focusing on provider affiliations and contracting entities—rather than solely relying on individual National Provider Identifiers (NPIs). By leveraging these additional data insights, organizations gain critical visibility into how healthcare providers, hospitals, physician groups, organizations, facilities, and healthcare systems are connected. This advanced approach helps streamline contracting efforts, network design, and network optimization.
Quest Analytics will highlight how performance intelligence can transform healthcare network strategies. By shifting the focus from individual National Provider Identifiers (NPIs) to contracting entities and provider affiliations, health plans gain a clearer understanding of network dynamics. This approach enables organizations to streamline contracting processes, achieve compliance objectives, and make more informed decisions. Learn how shifting from individual provider to contracting entity-level insights transforms network strategy and unlocks real business impact.
Speaker: Brent Sanders, Chief Commercial Officer, Quest Analytics®
Session Date: Wednesday, June 18, 2025, at 9:20 a.m.
Quest Analytics® Announces Strategic Integration Partnership with Arcadia
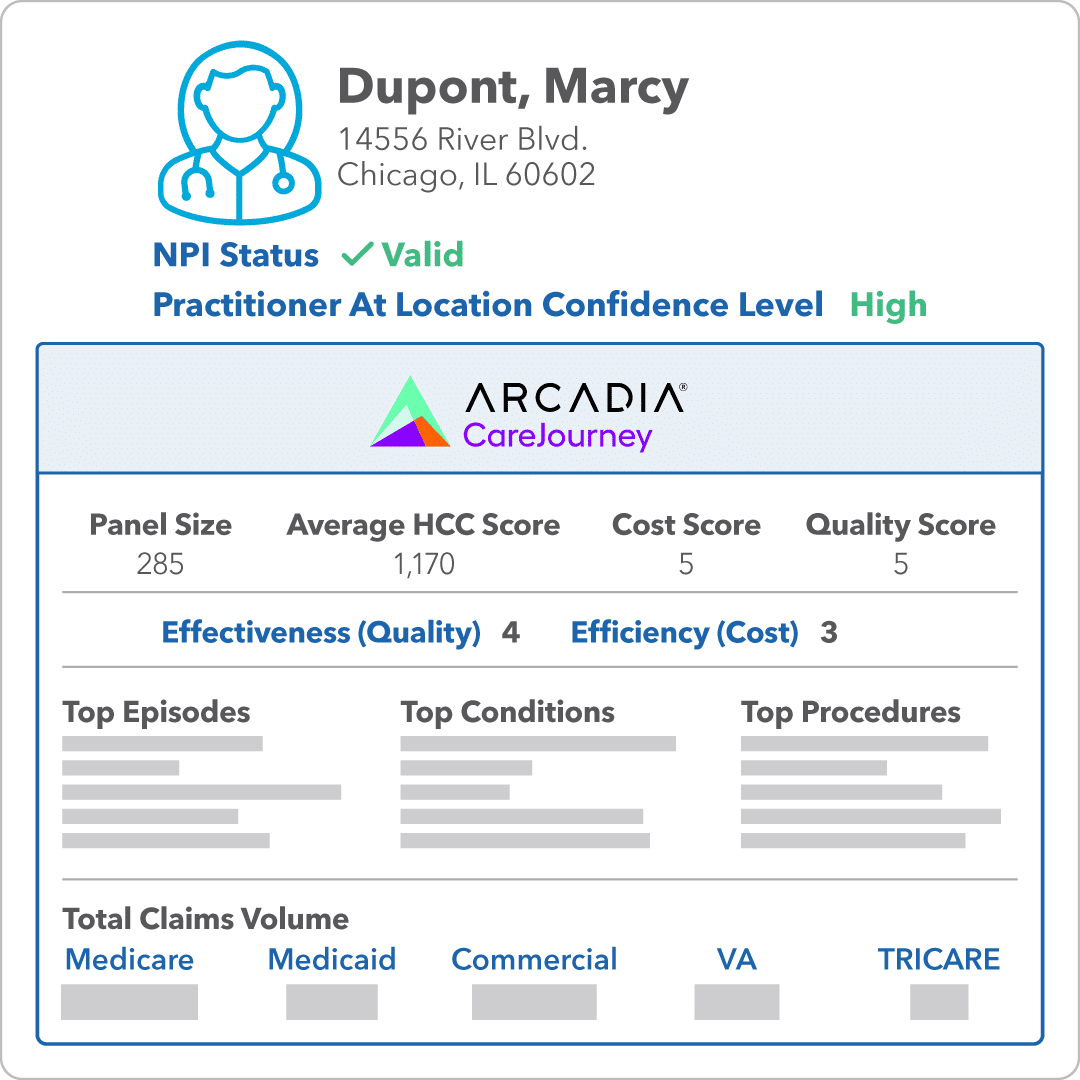
We’re pleased to share even more exciting news! In addition to QES Affiliation Insights, we announced our data integration partnership with Arcadia. This collaboration offers Quest Analytics clients enhanced physician-level intelligence within a single, streamlined platform to build high-quality, competitive networks.
Quest Enterprise Services® (QES®) Provider Claims Insights now integrates Arcadia’s CareJourney performance and cost measures, giving you deeper visibility into provider value across Medicare Fee-for-Service (FFS) Parts A, B, and D. Use these insights to:
- Pinpoint high-performing providers
- Optimize your contracting strategies
- Develop stronger, more competitive provider networks
It’s all designed to help you build smarter networks with ease and confidence.
Lunch & Learn Session
Session Title: Better Networks Require Better Data: Insights from a Survey of Health Plan Executives
When: Tuesday, June 17, 2025, at 12:25 p.m. – 1:35 p.m.
Despite significant investments in network design, health plans face unreliable data, limiting insights into provider performance and network competitiveness. Join this session to explore findings from a survey of 100 health plan executives, highlighting pervasive data issues and their impact on organizational priorities. Gain insights into claims-based validation, improving provider quality, enhancing competitive positioning, and how network design is critical to achieving success.
Speakers
- Kim Rogers, RN, MBA, Peak Health
- Bob Tavernier, Quest Analytics, LLC
Proven Solutions for Your Provider Network Management
Looking to simplify your workload? Let Quest Analytics take on the heavy lifting! Our solutions and dedicated team specialize in provider data accuracy and provider network adequacy for various lines of businesses, including Medicare Advantage, Medicaid and Commercial. Schedule a strategy session today and see how we can help you every step of the way.