QHP MARKETPLACE RESOURCES
Essential resources for issuers applying for QHP Certification to participate in the Marketplaces. Explore our growing library to find the latest news, tips, and support.
Featured QHP Certification News & Insights
Policy Brief: PY2026 QHP Certification Marketplace Final Rule
Updated to include the additional Network Adequacy and Provider Validation Requirements announced by CMS in May 2025. Policy Brief on the Final HHS Notice of Benefit and Payment Parameters for...
Executive Summary: New Rules for PY2026 QHP Certification
Updated: Includes the additional Network Adequacy and Provider Validation Requirements announced by CMS in May 2025. Prepare for the Plan Year 2026 QHP Certification Updates Staying compliant with the latest...
QHP Certification and Network Adequacy Review Timeline
Who doesn’t love a good calendar? We know we do. Whether you’re deep into network adequacy updates or juggling deadlines left and right, we’ve got your back. Our handy calendar...
Executive Summary: QHP Certification Data Validation Best Practices
Updated: Includes the additional Network Adequacy and Provider Validation Requirements announced by CMS in May 2025. Achieve Your QHP Certification Best Practices for a Successful QHP Application Getting your Qualified...
Network Adequacy and Provider Directory Accuracy Policy Updates
Federal and state regulators, along with lawmakers, are actively amending network adequacy and provider directory accuracy requirements while intensifying oversight. These changes have far-reaching implications for medical and ancillary plans....
CMS Provider Directory Pilot: What You Need to Know
CMS Qualified Health Plan (QHP) Directory Pilot The Centers for Medicare & Medicaid Services (CMS) launched a new provider directory pilot program with the Oklahoma Insurance Department (OID). Kate Deiters...
Episode: The Final 2026 Payment Notice for Qualified Health Plans
Episode: Health Policy Updates February 2025 The Final 2026 Payment Notice: Network Adequacy Updates for Qualified Health Plans Topics Covered The Final Notice of Benefit and Payment Parameters for 2026...
Find More Videos from Quest Analytics
Learn the latest news, insights, and strategies, from the experts at Quest Analytics. Explore our collection of provider network management videos on our YouTube channel.
🔔 Subscribe Today to be the first to access new content as soon as it’s released!
Listen to Our Latest Podcast Episodes
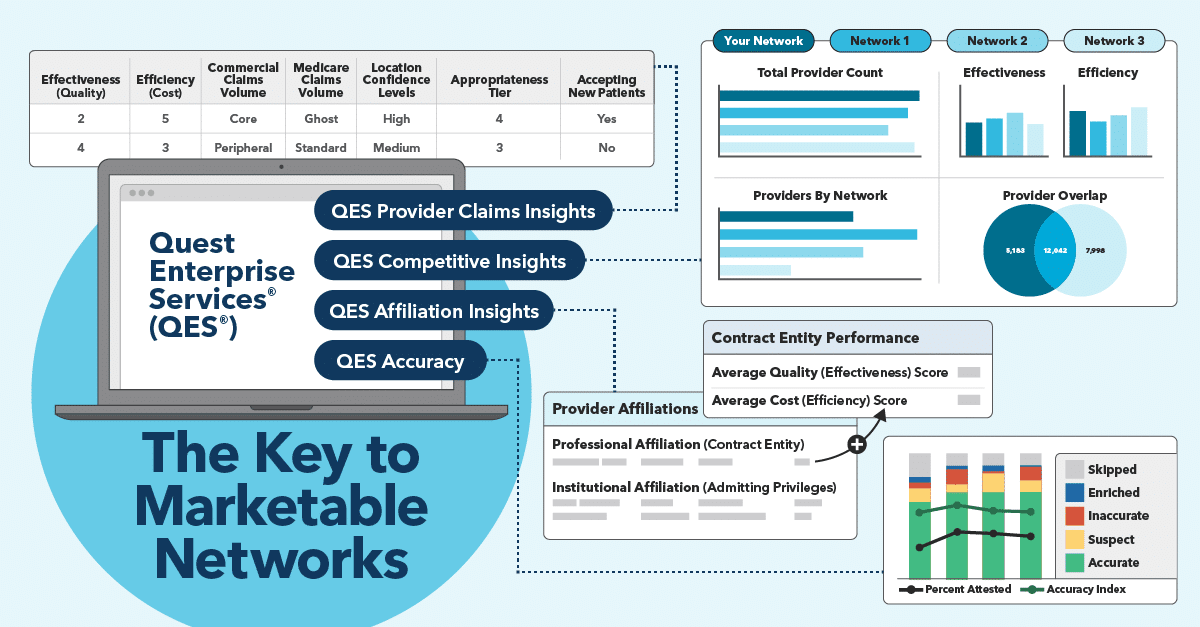
Network Performance News & Insights
Schedule Your Complimentary Strategy Session
Compliance isn’t our name, but it sure is our game! Learn how we can assist your efforts to make your provider data accurate and network adequate. Book a complimentary strategy session with a Quest Analytics expert to get started on your quest for success.