Payers & Plans
PROVEN PROVIDER NETWORK MANAGEMENT FOR COMMERCIAL HEALTH INSURANCE PLANS
Drive Performance, Win More RFPs, and Respond Confidently with Quest Enterprise Services
Take Your Provider Networks from Adequate to Competitive
In the highly competitive world of commercial insurance, making the right decisions about premiums, benefit design, and provider networks can have a significant impact on your success. Quest Analytics is here to support you every step of the way with our comprehensive solution, Quest Enterprise Services. Our proven provider network management solutions empower you to take your network from adequate to competitive, ensuring that you can meet the needs of your insured population and stay ahead in this ever-evolving industry.
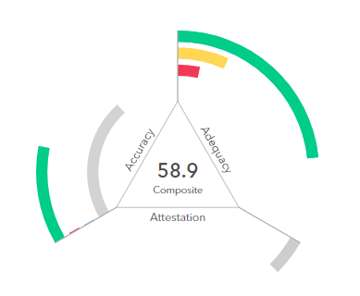
Measure, Manage, and Monitor Network Adequacy and Provider Data Accuracy
With Quest Enterprise Services, you have the power to measure, manage, and monitor the key metrics that drive the success of your provider networks. Our all-encompassing tools and actionable insights enable you to:
- Optimize Network Adequacy: Ensure that you have the right mix of healthcare providers to meet the needs of your members. This leads to better patient outcomes, increased member satisfaction, and improved network adequacy.
- Enhance Provider Data Accuracy: Get a clear understanding of the accuracy of your provider data and identify any gaps or errors that need to be addressed. This ensures that your network is up-to-date and in compliance with industry standards.
- Drive Performance: Leverage the insights gained from our services to make strategic decisions that drive performance and improve the overall efficiency of your provider networks.
- Win More RFPs: With a strong provider network and a demonstrated commitment to network adequacy and data accuracy, you’ll have a competitive advantage when responding to Requests for Proposals (RFPs).
- Confidently Respond to Accreditation Requests: Accreditation agencies like NCQA often require evidence of ongoing network performance measurement and management. With real-time insights into your network’s performance, you can easily respond to accreditation requests with confidence.


Optimize Your Dental and Vision Plans
When it comes to optimizing dental and vision plans, trust Quest Analytics to be your partner. Our comprehensive solutions, industry expertise, and innovative tools are designed to help you achieve your goals, whether it’s expanding your network or enhancing the quality of services. With our unique templates and actionable data insights, you can take your dental and vision plans to new heights.

Proven Methodology for Provider Data Accuracy
Provider data accuracy continues to take the industry by storm. As compliance with the No Surprises Act and other provider data accuracy regulations becomes increasingly crucial, we’re here to support you every step of the way. With our proven methodology and comprehensive services, Quest Enterprise Services Accuracy is designed to help you meet compliance and improve the accuracy of your provider data and networks.

Tailored Network Adequacy Templates for QHPs
When it comes to offering Qualified Health Plans (QHPs) through the Federally-facilitated Marketplace, having a network that meets the necessary network adequacy standards is paramount. That’s why we’ve developed network adequacy templates that are designed to help you save time while ensuring compliance with the requirements set forth by the Centers for Medicare & Medicaid Services (CMS).
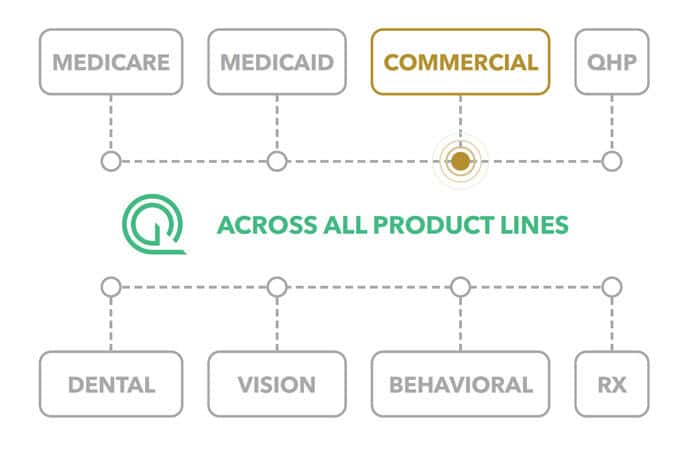
A LEGENDARY ENTERPRISE SOLUTION
By running all of your networks through a single provider network management platform, you’ll gain a better understanding of the strength of your network and the impact of your providers across business lines. You’ll create cross-departmental efficiencies, cut costs and have a realtime lens into how your network compares to the market.

Take the Next Step and Transform Your Provider Network Management
Quest Enterprise Services is your partner in achieving better network management, improved patient outcomes, and a competitive edge in the commercial health insurance market. Don’t miss out on the opportunity to optimize your provider networks and navigate the complex healthcare landscape with confidence.
Contact us today to learn more and schedule a demo of Quest Enterprise Services!








