Efficient and Compliant Provider Network Management
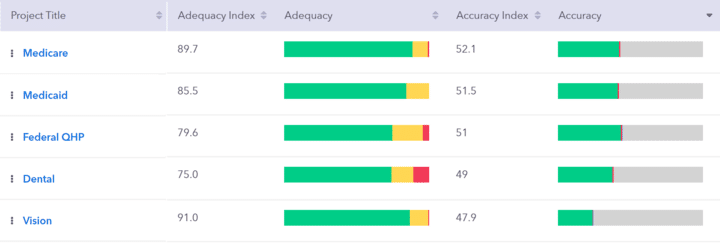
Measure Network Adequacy
Quest Enterprise ServicesTM measures network adequacy exactly the way regulators do—because CMS and many states use our tools in their audits, it finds the same gaps they would find.Measure Network Accuracy
Directory accuracy is measured by leveraging our National Database of primary-sourced, continuously updated provider data, along with other industry-known sources of truth. Letting you know what’s right, wrong and missing from your provider data allows you to focus resources and prioritize efforts on remediating the inaccuracies with the most impact.Manage & Monitor Together
And when you can measure these key performance indicators, you can finally manage them, efficiently, using powerful new tools to close adequacy gaps and correct provider directory accuracy issues. You can monitor performance over time to guide your management efforts. The result is not just compliant networks, accurate directories and better member experiences; it’s a stronger, smarter and more competitive organization overall.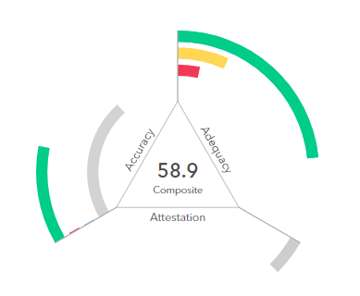

ACTIONABLE INSIGHTS ACROSS THE ENTERPRISE
Enterprise-wide management means more than connecting silos and streamlining the workflow.
It means giving everyone in your organization, regardless of product line or job function, access to the tools and insights they need to work more intelligently and more proactively.
And it means for the first time being able to ask—and answer—fundamental questions that will transform the way you work.
Network Adequacy + Provider Data Accuracy in One Platform
Measure network adequacy and provider data accuracy the way regulators do. Our tools are trusted by the Centers for Medicare & Medicaid Services (CMS) and State agencies. We offer pre-built Medicaid templates for many states based on the publicly available released standards.
Rest assured, our team actively monitors each state for updated guidance, ensuring our templates are up-to-date and accurate. With Quest Analytics, you can confidently evaluate your provider network and data, making informed decisions that align with regulatory requirements.
Quest Analytics State Templates
Quest Analytics has pre-built templates based on the standards & requirements for Medicare Advantage, Medicaid-Medicare, and an ever-growing list of state Medicaid programs. See which templates are available for you today!

Network Adequacy Compliance Monitoring and Audit Readiness Services
Measure and monitor your network access and adequacy in real-time shared across your organization.
Expansion Opportunities
Quest Enterprise ServicesTM provides you with several tools to help make strategic service area determinations with minimum effort. You can view the opportunity analysis of your current network in potential expansion areas, thereby allowing you to target areas that have the greatest return for the least amount of effort.
State-by-State RFPs
- Build targeted networks in a fraction of the time using our smart recruiting tools
- Identify quickly the best expansion opportunities based on revenue potential and recruitment lift to fill gaps
- Monitor and trend the progress and performance of each expansion opportunity providing full transparency across your organization
- Monitor and trend the progress and performance of each expansion opportunity providing full transparency for management
A LEGENDARY ENTERPRISE SOLUTION
By running all of your networks through a single provider network management platform, you’ll gain a better understanding of the strength of your network and the impact of your providers across business lines. You’ll create cross-departmental efficiencies, cut costs and have a realtime lens into how your network compares to the market.

Reduce Compliance Risks and Improve Network Quality
Discover comprehensive, efficient, and reliable Medicaid provider network management solutions. Our analytical tools, compliance expertise, and automation capabilities empower you to streamline network management, optimize quality, minimize risks, and enhance care for Medicaid beneficiaries. Contact us today to learn more.








