Quest Enterprise Services® (QES®)
Network Performance
Elevate Provider Networks with QES Network Performance Intelligence
Data-Driven Insights for Marketable, High-Performance Networks
As markets evolve, success hinges on adapting and driving sustained performance. QES® Network Performance solutions provide additional data insights and tools to build and optimize networks that consistently deliver value while preparing for future changes. With data-driven planning and strategic foresight, your network can meet today’s demands while positioning itself to seize tomorrow’s opportunities.
Network Optimization Built on Reliable Data
Gain a comprehensive view of provider efficiency, effectiveness, and quality. QES® Network Performance solutions enable you to identify strengths and pinpoint areas for improvement, providing actionable insights to enhance your network’s overall performance. By leveraging dependable, high-quality data, you can optimize your provider network to ensure it operates at peak efficiency.
Gain Competitive Insights to Drive Growth
Stand out in the market with strategies powered by actionable information. QES® Network Performance solutions allow you to identify opportunities for strengthening your competitive advantage, refining your organization’s unique value proposition, and driving quality improvements. Differentiate your network, attract more members, and deliver impactful care throughout the healthcare journey.
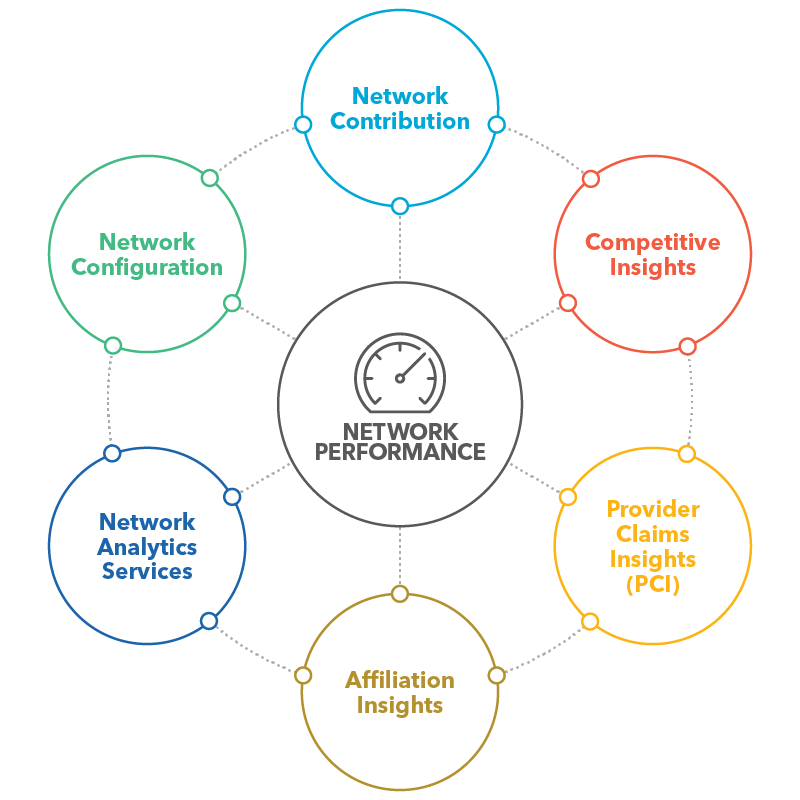
Provider Claims Insights
Provider Claims Insights offers a strategic edge in provider network management by incorporating a comprehensive national claims database. This premier solution grants you deeper data insights, encompassing cost, quality, and clinical activity metrics, empowering you to identify the top providers with ease.
Competitive Insights
Competitive Insights allows you to compare your network against competitors by providing access to key provider data. These insights enable you to make informed decisions when evaluating entry into new markets and optimizing existing networks, helping you drive strategic network differentiation and sustained competitive advantage.
Affiliation Insights
Affiliation Insights delivers a clear view into how providers and facilities align for contracting and clinical collaboration. By mapping organizational and practice relationships, this solution helps you identify contracting entities, assess provider affiliations, and evaluate clinical alignment. These insights enable smarter contracting strategies and more cohesive network design — helping you optimize performance, strengthen provider partnerships, and improve member experiences.
Network Analytics Services
Network Analytics Services are designed to empower your network management with actionable insights. We help you understand network utilization patterns, provider performance, and patient care trends by analyzing vast network data. Our services enable you to make data-driven decisions that enhance network efficiency and member outcomes.
Network Contribution
Network Contribution measures your health system’s impact on payer network adequacy. Viewing your provider footprint from a payer perspective can be a valuable tool in support of a payer negotiation or when evaluating expansion opportunities.
Network Configuration
Network Configuration helps you create and optimize networks faster. With network configuration, you define the optimal network in terms of access, provider performance, competitive overlap, or other KPIs. Quest will suggest that the providers to recruit to bring that network to life.
Discover More
Dive into additional resources for more information and valuable insights.
DELIVER ON TOMORROW’S GOALS BY PLANNING TODAY
We are committed to assisting you in your quest to achieve the Quadruple Aim – lowering costs and ensuring high quality of care while empowering patient and clinician experiences with actionable insights.
Schedule a consultative session with one of our health systems experts to discuss and determine your strategy.

Start a Conversation Today!