The Centers for Medicare & Medicaid Services (CMS) unveiled changes to the network adequacy application process for Medicare Advantage (MA) organizations. Whether you’re involved in compliance, market expansion, provider recruitment, or network management, these updates are crucial. Let’s break down these changes to help you understand the new process.
CMS Network Adequacy Reviews for Initial or Service Area Expansion Applications
MA organizations applying for an initial or expanded service area must demonstrate that their proposed provider network meets the network adequacy requirements for the pending service area during the application process.
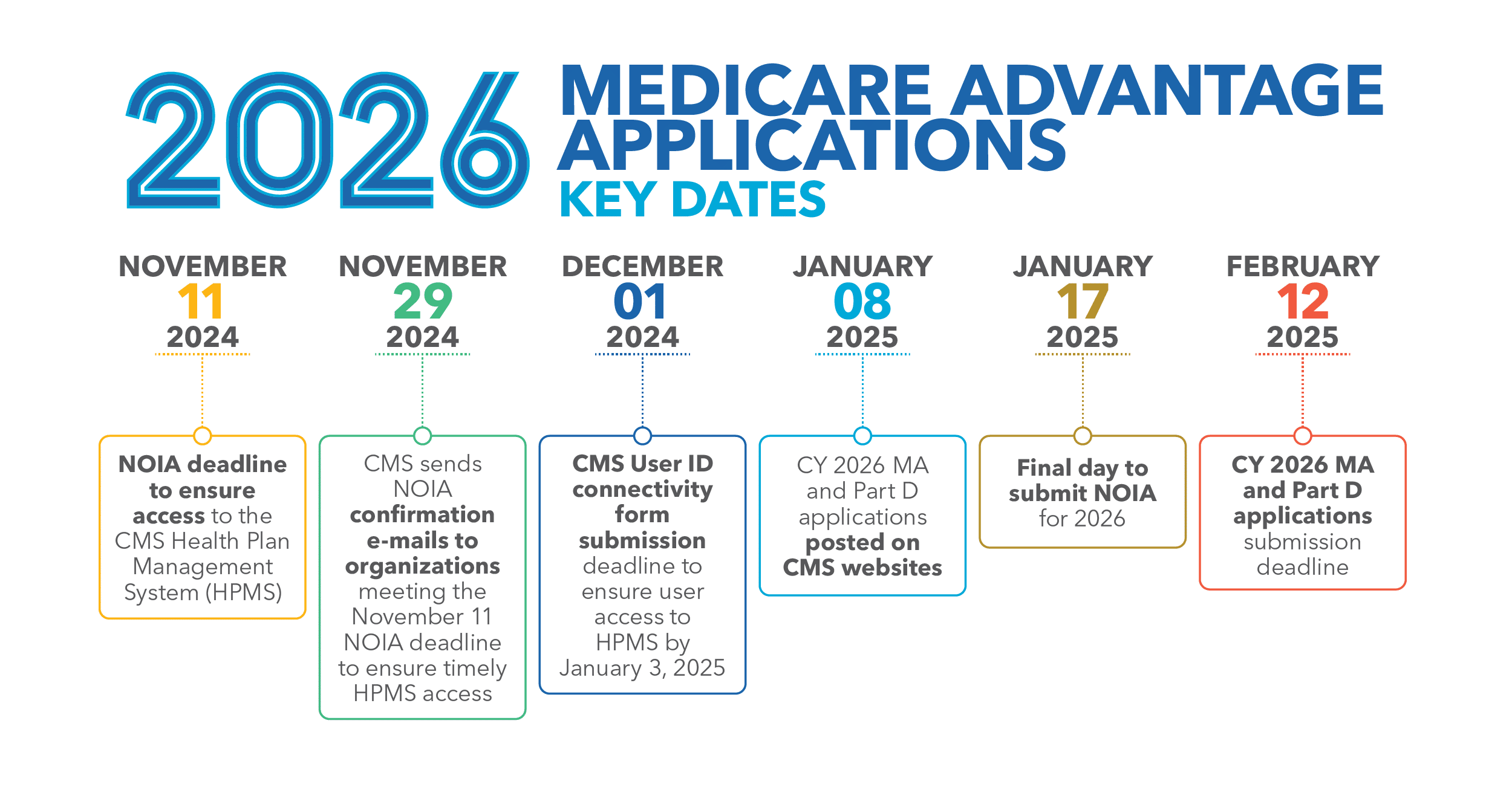
CMS CY 2026 Application Key Dates
Critical Deadlines for MA and Part D Applications

Changes to the MA organization Application Process
Proving Medicare Advantage Network Adequacy: HSD Table Submission
MA organizations must demonstrate that their proposed provider network meets the network adequacy requirements for the number of primary care providers (PCPs) and specialists within the designated time and distance standards.
To fulfill this requirement, MA organizations submit their provider and facility Health Service Delivery (HSD) tables to the Network Management Module (NMM) of the Health Plan Management System (HPMS). CMS will review the HSD tables to determine if the provider network meets the requirements.
Building Ahead: Timeline Adjustments
The proposed network must be adequate one year before it is live. This has a significant impact on MA organizations, as it forces them to adjust their timelines for future provider networks.
P.S. If you prefer video, watch this YouTube Video instead.
MEDICARE ADVANTAGE APPLICATION CHANGES
Scott Westover, SVP of Network and Regulatory Strategy at Quest Analytics, explains what the new network adequacy rules mean for Medicare Advantage Organizations.
Two Allowances For Initial or Service Area Expansion Applications
Building a compliant network a year ahead of the contract year is no small feat. Recognizing the time and effort required, CMS offers two allowances to help MA organizations meet network adequacy requirements.
Application Allowance 1: 10% Application Credit
Applicants can leverage the 10-percentage Point Credit towards the percentage of beneficiaries residing within the published time and distance standards for new or expanded service area applicants.
It’s important to note that the Application Credit only applies during the application process. Once the contract is live, the credit will no longer apply. The MA organization must meet full network adequacy requirements for the entire service area, beginning January 1 of the contract year.
Key Takeaways: Using the Application Credit
- The Application Credit only applies during the application process.
- The 10% credit will be automatically applied in HPMS and reflected on the MA organization’s Automated Criteria Check report.
- The 10 percent credit is in addition to other credits such as the Telehealth or Certificate of Need (CON) credits, if applicable.
- Once the contract is live, the credit will no longer apply.
- The MA organization must meet full network adequacy requirements for the entire service area, beginning January 1 of the contract year.
💡 Use Quest Enterprise Services® Medicare Advantage 10% Credit for Application Counties to quickly assess network adequacy for your proposed counties with the new 10% application credit today.
Application Allowance 2: Letters of Intent to Contract
Applicants are allowed to submit a Letter of Intent (LOI) to contract in place of a signed provider contract at the time of application and for the duration of the application review to meet network standards. The intention is to give applicants seeking to expand into a new market the opportunity to reach the threshold for network adequacy while still finalizing contract details.
Important Considerations for MA organizations Using Letters of Intent
Keep two aspects in mind if you are considering using a Letter of Intent.
Conversion into Full Contract by January 1
MA organizations must ensure that the Letter of Intent is fully executed contracts before January 1, of the go-live date.
Participation in the Triennial Review
MA organizations that use Letters of Intent for the application of a new or expanded service area must participate in a Triennial Network Adequacy Review the first year the plan is operational in its new service area.
Key Takeaways: Using Letters of Intent
- The Letter of Intent is only for Initial or Service Area Expansion counties.
- Have a process and plan to assess your network for compliance regularly and after every mid-year termination.
- Don’t underestimate the effort and time required to convert to a full contract. Each Letter of Intent must be signed per unique NPI.
- If a Letter of Intent is incorrect, the MA organization will have 10 days to correct and resubmit to CMS.
- When resubmitting, all other Letters of Intent must be included with the corrected one.
3 Steps to Help You Prepare for Your Medicare Advantage Application
Step #1: Review and Validate the Provider Network
Before your network submission, it’s essential to review your data. Pay special attention to the new behavioral health specialties in your HSD tables. Make sure they’re accurately listed and that your network meets the requirements for network adequacy. This step ensures that you have the updated and complete information necessary for a successful submission.
Step #2: HSD Tables Must Match Your Provider Directory
To avoid data discrepancies or compliance issues, ensure that your provider directories and HSD tables match. Take the time to compare and cross-check the data in both sources. This way, you can be confident that your provider directories accurately reflect the information listed in your HSD tables.
Step #3: Limit Provider Locations in HSD Tables
When it comes to your HSD tables, it’s important to set limits on the number of locations listed for each provider. To stay in compliance and avoid any concerns, ensure that providers in your HSD tables are limited to 5-10 locations.
💡 Looking for network submission tips? Check out: 8 Data Tips for Medicare Advantage Network Adequacy Reviews.
Maximizing Compliance and Success
Stay updated on the recent updates to network adequacy oversight by CMS and understand how it impacts MA organizations. By ensuring compliance, meeting new requirements, and proactively addressing network adequacy, your organization can provide top-quality care to beneficiaries while also achieving goals of compliance, expanding in the market, and recruiting providers. Quest Analytics® is here to assist you throughout this process, offering expert guidance and actionable insights to help you optimize your provider networks and ensure compliance. Have questions? Reach out to us today and let our experts guide you.
Proven Solutions for Your Provider Network Management
Looking to simplify your workload? Let Quest Analytics take on the heavy lifting! Our solutions and dedicated team specialize in provider data accuracy and provider network adequacy for various lines of businesses, including Medicare Advantage, Medicaid and Commercial. Schedule a strategy session today and see how we can help you every step of the way.