Medicare Advantage (MA) Organizations applying for initial, or service area expansion can use Letters of Intent in place of a signed contract to help meet network adequacy requirements while going through the application process. The intention is to give applicants seeking to expand into a new market the opportunity to reach the threshold for network adequacy while still finalizing contract details. As part of an allowance during the network adequacy review process, applicants must notify CMS of their use of Letters of Intent to meet network standards. In this article, we provide answers to frequently asked questions related to the use of Letters of Intent by Medicare Advantage Organizations during the application process.
Letter of Intent During the Application Process
Q: Why do Medicare Advantage Organizations use Letters of Intent during the application process?
A: Letters of Intent allow Medicare Advantage Organizations to meet network adequacy requirements while applying for initial approval or service area expansion. It can be challenging for Medicare Advantage Organizations to build a complete provider network before receiving a Medicare Advantage contract. Letters of Intent serve as placeholders for signed contracts during this period.
Explore how Quest Analytics assists Medicare Advantage Organization Provider Network Management to meet network adequacy and provider data accuracy requirements.
Q: What is the purpose of using Letters of Intent during the application process?
A: The purpose of using Letters of Intent is to demonstrate the Medicare Advantage Organization’s commitment to establishing a compliant provider network before the formal contract with the provider is signed. It allows applicants to meet the network adequacy threshold while finalizing contract details.
Q: Are there any product types exempted from using Letters of Intent for network adequacy?
A: Yes, it’s important to note that the use of Letters of Intent for network adequacy is specific to Medicare Advantage Organizations. It does not apply to certain product types, including Medicare/Medicaid Plans (MMPs), section 1833 cost plans, non-network private fee-for-service (PFFS) plans, and network-based medical savings account (MSA) plans.
Q: Is there a deadline for converting a Letter of Intent into a full contract?
A: Yes, by January 1, all Letters of Intent must be converted into full contracts to count toward meeting network adequacy requirements. Medicare Advantage Organizations must ensure that all Letters of Intent are formalized into signed contracts before this deadline.
Q: Are Medicare Advantage Organizations required to participate in the Triennial Review if they use a Letter of Intent?
A: Yes, CMS requires any Medicare Advantage Organization that uses a Letter of Intent with its application to participate in the Triennial Review. This review is conducted during the first year of the plan’s operation in the new service area.
Medicare Advantage Applications and Letters of Intent: Process and Timelines Explained
Wondering when and how to submit Letters of Intent during your Initial or Service Area Expansion application? Watch this clip from our recent What’s New Webinar where Roxanne Butts, Client Services Consultant at Quest Analytics, walks you through the operational instructions and submission timelines.
Q: When can applicants submit Letters of Intent?
A: Letters of Intent can be submitted in two situations.
1. Letters of Intent can be submitted in response to a Deficiency Notice.
ICYMI: If an applicant marks “Y” in the initial application submission, they will receive an error.
2. Letters of Intent can be submitted in response to a Notice of Intent to Deny.
Tip: Only new or corrected Letters of Intent should be submitted in response to a Notice of Intent to Deny.
Q: Can Letters of Intent be used with active and expansion counties?
A: No, Letters of Intent only apply to Initial or Service Area Expansion counties.
Q: Can Letters of Intent be used for active counties during Triennial Network Adequacy Reviews?
A: No, Letters of Intent should not be used for active counties during a Triennial Network Adequacy Review.
Q: Which providers should be included in the initial HSD table submission with the Application?
A: Only contracted providers should be included in the February submission with the Application.
Q: Should Letters of Intent be included in the first Health Service Delivery (HSD) table submission?
A: No, Letters of Intent should not be included with the first HSD submission in February.
Q: Can Letters of Intent be submitted for individual and group level practitioners?
A: Yes, applicants can submit Letters of Intent at two levels:
- Individual Provider Letters of Intent
- Group Practice Letters of Intent
Q: How should applicants notify CMS they intend to use Letters of Intent?
A: When responding to the Deficiency Notice or Notice of Intent to Deny, applicants must mark “Y” in the HSD table column, “Letter of Intent? (Y/N)”, to let CMS know they wish to use a Letter of Intent to meet network adequacy.
Tip: Quest Enterprise Services®(QES®) Medicare Advantage template offers a dedicated column for efficiently identifying and monitoring providers with a Letter of Intent in your pending counties.
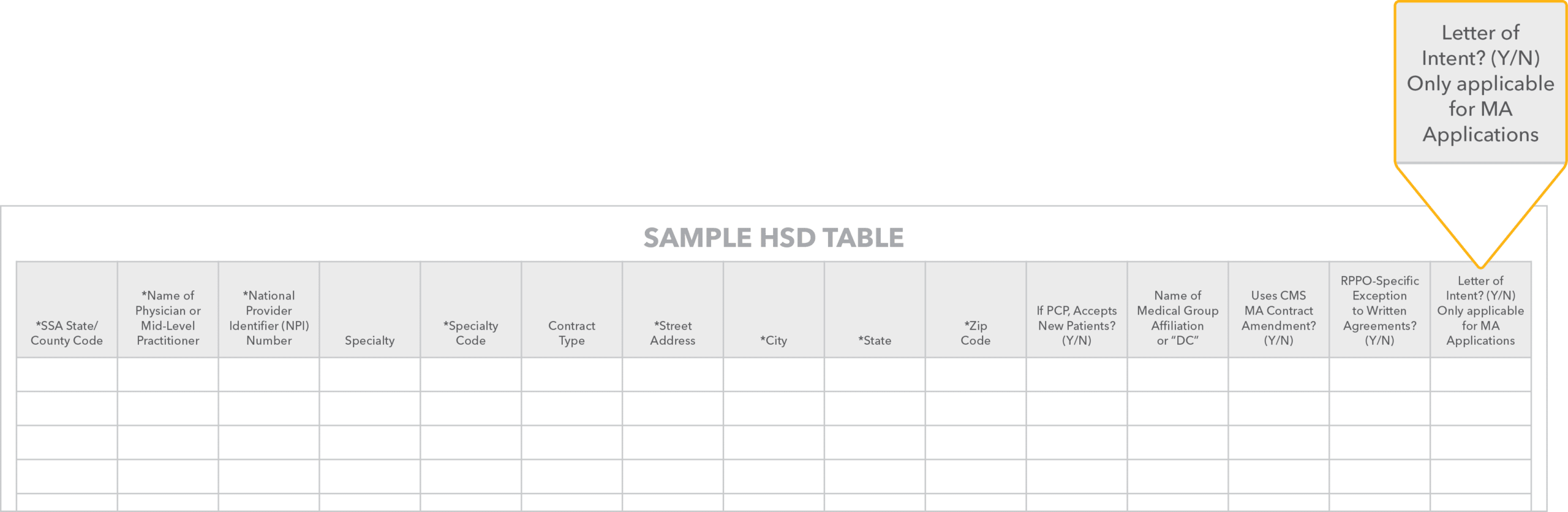
Q: Are there specific requirements for submitting Letters of Intent at the Individual Provider Level?
A: Yes, as a resubmission in response to a Deficiency Notice or a Notice of Intent to Deny, applicants using individual level Letters of Intent, the first step is to mark a “Y” in the column, “Letter of Intent? (Y/N)” in the HSD table for each provider they’re using a Letter of Intent.
Second, applicants must upload a one-page Letter of Intent in PDF format for each National Provider Identifier (NPI) identified in each county and specialty combination where the Letter of Intent is indicated in the HSD table. The one-page Letter of Intent PDF must be in the form CMS specified and include the following items.
- Letterhead: The Letter of Intent must be on the Medicare Advantage Organization’s official letterhead.
- Signatures: Signatures from both the Medicare Advantage Organization and the provider or facility.
- Statement: A statement that the applicant and the provider have started negotiations or intend to negotiate for the provider to participate in the applicant’s network of contracted providers.
Example Template:
One-Page PDF Letter of Intent
See an example of a template for the one-page PDF Letter of Intent. Download here.
Q: Are there specific requirements for submitting Letters of Intent at the Group Practice Level?
A: Yes, as a resubmission in response to a Deficiency Notice or a Notice of Intent to Deny, Medicare Advantage Applicants using Group Level Letters of Intent, the first step is to mark a “Y” in the column, “Letter of Intent? (Y/N)” on the HSD table for each provider they’re using a Letter of Intent.
Second, applicants must upload a one-page Letter of Intent in PDF format for the Group Practice. The one-page Letter of Intent PDF must be in the form CMS specified and include the following items.
- Letterhead: The Letter of Intent must be on the Medicare Advantage Organization’s official letterhead.
- Signatures: Signatures from both the Medicare Advantage Organization and the Group Lever Provider.
- Statement: A statement that the applicant and the provider have started negotiations or intend to negotiate for the provider to participate in the applicant’s network of contracted providers.
Tip: Group Level Letter of Intent submissions must use the Group to NPI Matrix Template with their submission. Only submit one matrix per submission round.
Third, the applicant must submit one Group Level Letters of Intent Excel spreadsheet per zip file containing the Letter of Intent matrix which includes the following columns.
- Medical Group Practice Name: The corresponding group-level provider or facility name for each group-level Letter of Intent submitted.
- Individual NPI Number: Individual provider NPIs listed in this column must also be included in the HSD file submission.
- Letter of Intent Filename (Group Level): must include the group level provider or facility name. For example, H0001_Sample Health System.pdf
Q: Can multiple Letters of Intent files be uploaded?
A: Yes, multiple Letter of Intent files can be uploaded.
Q: Are there any limitations on file sizes when uploading Letters of Intent in HPMS?
A: Yes, it is important to note that files that are too large may not be able to be uploaded with the submission in the Health Plan Management System (HPMS). The uploaded file should be one zip file, not exceeding 500MB in size.
Q: What happens if CMS finds the Letter of Intent invalid?
A: In cases where CMS deems a Letter of Intent invalid, the applicant can correct the letter and resubmit it along with their response to the Notice of Intent to Deny.
Q: Where can I find detailed upload instructions for the Network Management Plan?
A: For specific upload instructions, we recommend reviewing the Network Management Plan User Guide or reaching out to your CMS representative.
You can also submit questions on Medicare Advantage and Cost Plan Applications to the Division of Medicare Advantage Operations.
Please note that the guidance in this article does not apply to certain product types, including Medicare/Medicaid Plans (MMPs), section 1833 cost plans, non-network private fee-for-service (PFFS) plans, and network-based medical savings account (MSA) plans.
How does Quest Enterprise Services Solve for the Letter of Intent?
Quest Enterprise Services® (QES®) Adequacy dramatically simplifies the management of Letters of Intent. QES provides a compliant Medicare Advantage Network Adequacy template with all the necessary fields for HSD tables and Letter of Intent management, including a dedicated column that allows you to track which providers are using a Letter of Intent in your pending counties. Saving you time and effort, QES automates the entire process, eliminating the need for separate analyses or manual calculations. Manage your network with ease by scheduling a strategy session with one of our network experts to learn more.
Related Articles on Medicare Advantage Network Adequacy and Provider Directory Accuracy
Know Your Data, Grow Your Business
Get a complimentary strategy session with a Quest Analytics expert to learn how we can help you maintain network adequacy, improve data accuracy and achieve astonishing efficiencies.