FIVE TAKEAWAYS FROM OUR WEBINAR
Watch: Designing and Building Clinician Networks That Address Social Determinants of Health
As clinicians and payers take on increasing risk for patient outcomes, it is essential that leaders consider the effectiveness of their networks as well as the accuracy of their clinician directories to ensure they are adequately serving their members. Modern Healthcare and Quest Analytics partnered together to host a panel of healthcare experts discussing the importance of considering social determinants of health in building adequate and accurate provider networks. Here are the key points to know.
1. Improve management, priorities, coverage, and function of networks
Historically, payers have considered network management, adequacy, and accessibility as transactional functions in their efforts to build provider relationships while meeting regulatory and accessibility standards. The focus must shift to the creation of blueprints for networks of clinicians that are truly built for the communities they serve and the consumers within those communities. In order to build networks that are responsive to community needs, organizations need to recognize that the adequacy of the network is inextricably linked to the accuracy of the clinician data. With clear analytics, organizations can strategize to build efficient and effective networks that are far more impactful than large PPO broad access networks that use accessibility standards merely as a regulatory criterion.
2. Define Social Determinants of Health (SDoH)
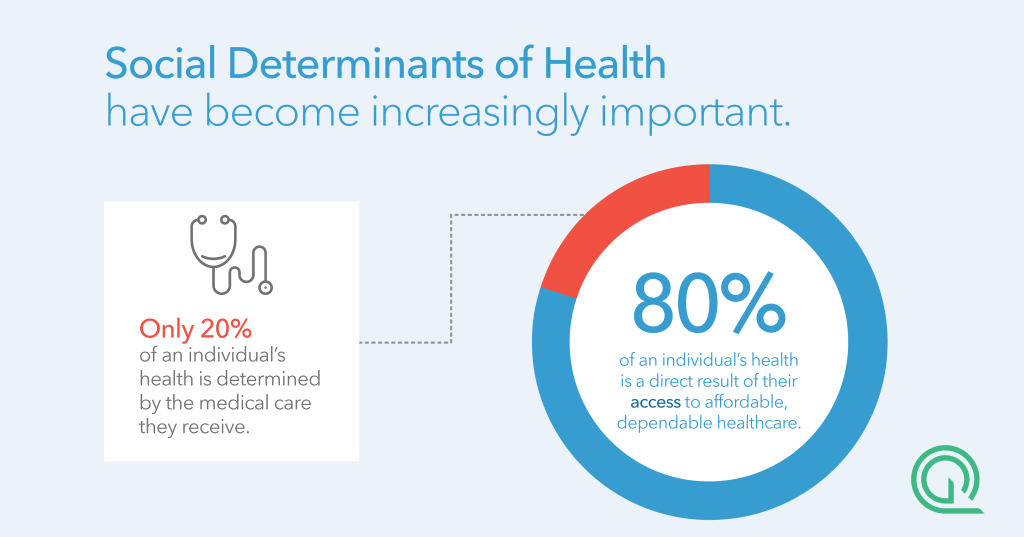
In a poll of webinar participants, 60 percent selected social and community context as the No. 1 social determinant, followed by healthcare access and quality. Social determinants have become increasingly important—research shows that only 20 percent of an individual’s health is determined by the medical care they receive. The additional 80 percent is a direct result of their access to affordable, dependable healthcare—including behavioral healthcare—as well as their environment, including transportation, food security, nutrition, loneliness and isolation, especially among seniors. These and other factors, especially during a pandemic, affect health outcomes. The goal is to modify these percentages through data-driven care.
3. Drive regulatory data to improve SDOH
Healthcare costs continue to place an enormous burden on families. A more thorough understanding of patient and provider data, and how that data meshes with regulators’ priorities, will help decrease costs for patients. The most important regulator driver of SDOH is access to providers, according to a poll of webinar participants. Although policymakers are aware that reducing the impact of negative social determinants, such as poor access to healthcare, can be a useful strategy in reducing long-term health care costs, they understand that more help is needed.
4. Emphasize the importance of primary care
Whether delivered virtually, over the phone, in a medical facility or in the home, the most effective and impactful way to get a consumer connected to the healthcare system is through primary care. At best, a patient’s primary care provider is a trusted adviser who has the expertise and forward vision to help patients connect with others in the system who can be of the most assistance. All efforts should be made to bring tools, capabilities and resources to primary care practices in an effort to make providers more useful to their patients and more involved in their care.
5. Play a larger role in expanding and improving the resources of patients
Since the health and well-being of those served by the healthcare community is directly impacted by the resources—food, transportation, and more—available to those patients, it’s important that healthcare organizations play an advisory—and in some cases active—role in addressing those needs. With insights and access to data that informs an organization about more than simply whether their network is adequate, healthcare organizations can work in tandem with community organizations, outside investors and other societal factions to manage, monitor, and measure a patients’ access to their own unique care. If done correctly, these insights will then play a direct role in a community’s overall access to care and health in general.
More Resources At Your Fingertips
Access the full webinar to hear how healthcare organizations are combining social determinants of health (SDOH) with network adequacy standards to deliver better patient care. Watch: Designing and Building Clinician Networks That Address Social Determinants of Health