Managing a Medicare-Medicaid Plan (MMP) provider network is no small feat, and deadlines can sneak up on you quickly. To ensure you stay ahead, we’re here to provide all the essential details you need to know for the upcoming network submission.
Network Submission Due Date Reminder
Key Dates and Times
Let’s dive straight into the specifics. The initial deadline for the 2024 MMP Provider Network Submission is September 17, 2024, at 8 p.m. E.T. Make sure to submit your network data through the CMS Health Plan Management System (HPMS) before this time.
HPMS Gate Opening
The MMP Network submission in the HPMS Network Management Module (NMM) will be open from September 3, 2024, at 9 a.m. E.T., until September 17, 2024, at 8 p.m. E.T. You have a two-week window to complete your network submission.
Pro Tip: Avoid last-minute submissions. Learn how Quest Enterprise Services® can assist you in staying review-ready and compliant-confident.
MMP Provider and MMP Facility Table Templates: What You Need to Know
Instructions and Template Overview
With the deadline in mind, let’s discuss the necessary steps for a successful submission. You should include all contracted providers within and outside the service area who will be available to serve county beneficiaries.
The MMP Network Submission requires you to submit Health Service Delivery (HSD) tables for the service area reflected in the CMS HPMS. Use the current provider and facility templates located in HPMS to submit your HSD tables.
- MMP Provider Table Template
- MMP Facility Table Template
Reminder: Your network must include providers for the two new behavioral health provider specialty types: Clinical Psychology and Clinical Social Work.
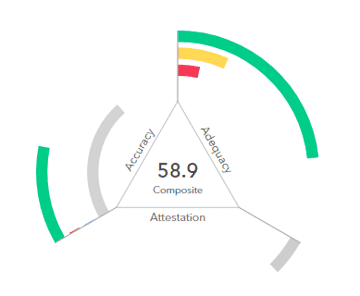
Automated Criteria Check Reports
Assessing the Status of Your Network
After you’ve submitted your MMP HSD tables, you’ll receive an Automated Criteria Check (ACC) report. Think of it as your network’s report card. It will indicate which providers and facilities meet network adequacy standards and highlight any deficiencies that need addressing.
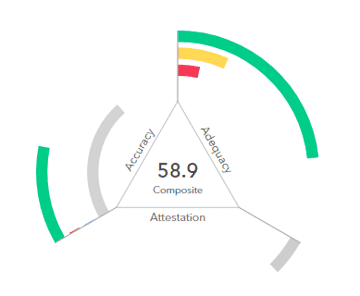
Reminder: CMS will apply rounding for the MMP network submission to results of 89.5% or higher. Be sure your network meets or exceeds this threshold.
MMP Annual Network Submission HSD Exception Request Template
Addressing Network Deficiencies
If your network shows deficiencies, don’t worry. You can submit an exception request using the current MMP Annual Network Submission HSD Exception Request template.
When submitting an exception request, make sure to provide comprehensive information and documentation to support your case. The template will guide you through the specific requirements to ensure completeness.
Expediting the Process. Eliminating Exception Requests.
Discover how Quest Enterprise Services Exceptions helps a regional health plan eliminate the need for exception requests. Download Now.
Key Requirements to Keep in Mind
Consider the following when submitting your MMP Annual Network Submission HSD Exception Request.
Exception Request Timelines
Exception Request submissions in HPMS NMM will be open from September 18, 2024, at 9 a.m. E.T. until October 2, 2024, at 8 p.m. E.T. Ensure submissions are within this window for consideration.
Use the Correct Template
Always use the current MMP Annual Network Submission HSD Exception Request template. Requests submitted using the Medicare Advantage application template or previous versions won’t be accepted.
CMS Communication
Stay tuned for HPMS email notifications from CMS, indicating the completion of the exception request review and the availability of updated ACC reports in HPMS. Look out for automated emails from CMS when the NMM gates reopen for resubmissions.
Stay Review-Ready: Medicare-Medicaid Plan Network Adequacy Compliance
Evaluate, pinpoint, and advance with unwavering confidence. Download your CMS Medicare Network Adequacy and Provider Data Accuracy Audit toolkit to maintain an unbeatable edge in Medicare-Medicaid plan network adequacy compliance. Download Now
You're Ready for the Upcoming MMP Network Submission
With the essential information at your fingertips, it’s time to prepare for the upcoming MMP Network submission. Mark your calendar, use the provided templates, and review your network meticulously. Remember, we’re here to support you every step of the way. Good luck, and may your networks remain strong and compliant!
CMS Resources
- Medicare-Medicaid Plan (MMP) Application & Annual Requirements are available on the CMS website.
Discover More Strategies for Success for Medicare-Medicaid Plans
Proven Solutions for Your Provider Network Management
Looking to simplify your workload? Let Quest Analytics take on the heavy lifting! Our solutions and dedicated team specialize in provider data accuracy and provider network adequacy for various lines of businesses, including Medicare Advantage, Medicaid and Commercial. Schedule a strategy session today and see how we can help you every step of the way.