Federal and State Regulators
Quest Enterprise Services® for Federal and State Regulators Network Adequacy and Provider Directory Accuracy
Discover Why Over 30 Regulatory Agencies Trust Quest Analytics®
Industry-Leading Network Adequacy and Provider Directory Accuracy Solutions
For nearly 20 years, we have been the trusted partner for regulators who monitor network adequacy and provider directory accuracy. Our long-standing contractual relationships with the Centers for Medicare & Medicaid Services (CMS) and state agencies have set industry standards for regulating plans, giving us an understanding of the intricacies involved in health network assessments.
Trusted by Regulatory Agencies Nationwide
More than 30 state agencies and independent review organizations, including the Departments of Insurance and Health and Human Services, partner with us. Our advanced analytics and innovative solutions enable these entities to fulfill their oversight responsibilities with unprecedented efficiency and effectiveness.
Our partnerships extend beyond network monitoring platforms. We actively engage with federal policymakers, State Insurance Commissioners, and State Medicaid Directors to collaboratively enhance network adequacy and provider directory accuracy. By leading the integration of emerging measures such as enhanced network adequacy and network adequacy telehealth credits, regulators can implement additional strategies that expand care access in their communities.
Quest Enterprise Services® for Regulators
Quest Enterprise Services® elevates the capabilities of federal and state health plan regulators in overseeing network adequacy and provider directory accuracy. Our platform transcends traditional oversight methods, delivering unparalleled insights to optimize regulatory processes. Key functions are automated, enabling significant time and resource savings while enhancing healthcare access.
Streamline Network Assessment And Oversight
Streamline network assessments with our automated solution, equipped with built-in network adequacy standards and requirements. Quest Enterprise Services® continually evolves to include metrics such as enhanced network adequacy, geographic distance calculations, telehealth credits, ghost provider analysis, and comprehensive provider claims activity monitoring. Our solution also evaluates providers operating at multiple locations. Additionally, we empower you to improve your provider directory audits and implement strategic improvement initiatives, strengthening your regulatory oversight and operational efficiency.
Advanced Issuer Comparative Analysis
A distinctive feature of Quest Enterprise Services® is the ability to compare multiple health plans simultaneously. With this functionality, you can evaluate and contrast issuer network adequacy and performance. Such comparative analysis empowers data-driven decisions that enhance network adequacy and health plan quality.
Customizable Regulatory Standards
Recognizing the unique needs of each regulatory body, Quest Enterprise Services® offers customization options to align with specific regulatory review standards. Collaborating closely with your team, we tailor network standards to meet your requirements, ensuring precise alignment with your regulatory goals.
Enhance Consumer Protection and Public Policy
Quest Enterprise Services® offers unparalleled visibility into key information such as provider availability in the market. Leveraging real-time data trends provides you with the information you need to give to legislators who are shaping policies that are responsive to current and future market dynamics.
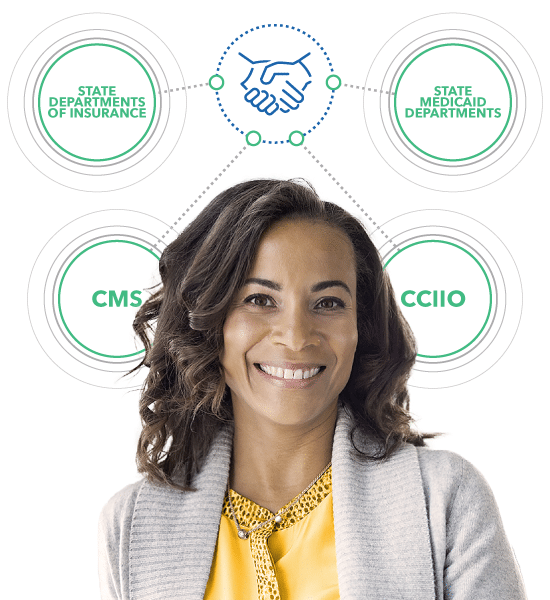
Solutions for All Programs
Leveraging a strategic approach to regulatory compliance across healthcare landscapes, we form pivotal partnerships with key entities such as CMS, the Center for Consumer Information and Insurance Oversight (CCIIO), state agencies, and state-based exchanges to deliver reliable solutions tailored for Medicare Advantage, Medicaid, and Federal and State Marketplaces.
Our long-tenured partnership with CMS includes the necessary tools and solutions essential for thorough network oversight and the evaluation of network adequacy for Medicare Advantage Part C & D.
CMS conducts annual health plan network adequacy evaluations, as well as triennial reviews of participating health plans, to verify the accuracy of submitted network data. To streamline this process, CMS relies on Quest Analytics’ solutions to facilitate the review of Health Service Delivery (HSD) tables from participating plans.
Additionally, we work with CMS and regulators to help determine feasible regulations based on geography and available providers by specialty – helping to eliminate unnecessary exception fillings that take up scarce resources.
Our partnership with CMS underscores the power and significance of our relationship in the provider network compliance and management industry, setting a standard for ensuring compliance and enhancing the quality of care for the population served.
We partner with dozens of State Medicaid Agencies to provide the solutions they need for network adequacy evaluations and oversight. Additionally, we assist them with the development and implementation of quantitative network adequacy standards and provider directory accuracy requirements. Given Quest Analytics’ knowledge of evidence-based quantitative network adequacy standards, our strong relationships with network adequacy leaders inside CMS, and our contractual relationships with Managed Care Organizations, Quest Analytics is in a strong position to offer expert assistance to any State in the development of standards.
Federally-facilitated Marketplace
We partner with the Center for Consumer Information and Insurance Oversight (CCIIO), to deliver targeted solutions and services that assess network adequacy for Qualified Health Plan (QHP) certification. This is vital as 29 states participate in the Federally-facilitated Marketplace and must comply with network adequacy requirements. Our offerings enhance the agency’s ability to monitor compliance effectively while simultaneously deepening its insight into market trends and behaviors.
State-based Exchanges
We partner with policymakers and regulators on State-Based Exchanges, offering solutions and services to assess network adequacy for Qualified Health Plan (QHP) certification. Our expertise streamlines the transition to align state network adequacy requirements with Federal standards while enabling a thorough understanding of the optimal requirements for the state. Agencies can enhance their compliance monitoring capabilities and gain deeper insights into market trends and behaviors.
Solutions for Regulators
With Quest Enterprise Services®, your agency has the actionable insights, resources, and tools needed to help manage and monitor provider networks. Schedule a consultation with our Regulatory Team today to learn how Quest Enterprise Services® can help meet your program oversight needs.

Join Our Regulator Exclusive Webinars
Connect with fellow regulators and policymakers in our Regulator Exclusive webinars, designed to address critical issues such as network adequacy and provider data accuracy. Learn about advanced strategies, share valuable insights, and collaborate to drive meaningful changes in the healthcare industry.
For more information, contact our Regulatory Team at Regulatory@questanalytics.com.
Discover More
Dive into additional resources for more information and valuable insights.
Supporting Your Efforts in Delivering Quality Healthcare
As you work to ensure that health plans in your state offer affordable and quality healthcare, Quest Analytics® is here to assist you. Contact us with any questions or to discuss how we can support your efforts.

Start a Conversation Today!