Payers & Plans
Proven Provider Network Management for Health Insurance Exchanges
Simplifying Provider Network Management, Network Adequacy Compliance, and QHP Certification
Providing Comprehensive Solutions for Health Insurance Issuers
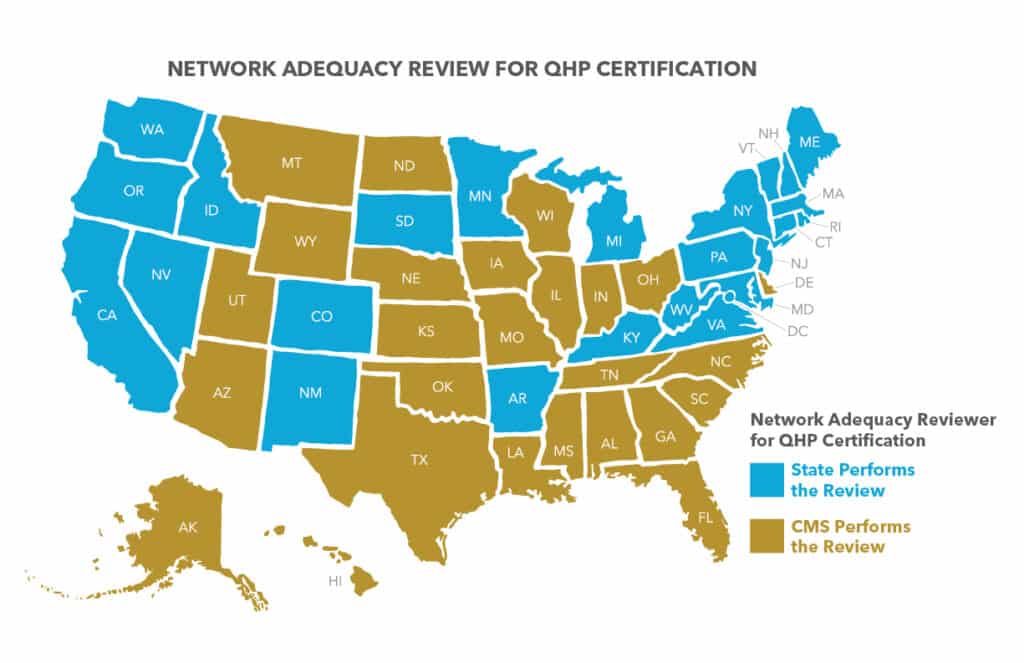
Health insurance issuers face a unique set of challenges when it comes to provider network management, network adequacy compliance, and quality health plan (QHP) certification. That’s why we offer specific services to help insurance issuers on the Federally-facilitated Exchange (FFE), State-Based Exchanges (State Exchanges), or State-Based Exchanges using the Federal Platform (SBE-FPs) every step of the way.
Streamline Compliance with Quest Enterprise Services Templates
Our pre-built templates, such as the CCIIO QHP FFE Network Adequacy Template for QHP certification and Custom Templates for State-Based Exchanges, are designed to help you evaluate your network with compliance standards. These templates come pre-loaded with essential criteria, saving you time and effort.
- Continuously monitor your network to ensure network adequacy compliance
- Quickly identify deficiencies in your provider network
- Easily understand what is right, wrong, and missing in your provider data
- Streamline you provider recruitment efforts

Quest Enterprise Services Custom Network Adequacy Templates
Quest Analytics has pre-built templates based on the standards & requirements for an ever-growing list of state agencies. See which templates are available for you today!
Quest Enterprise Services CCIIO QHP Network Adequacy Template
Our CCIIO QHP Network Adequacy template is built according to the federal requirements for specialty type, time and distance standards set forth by CMS.
Why Choose Quest Analytics?
Network Adequacy Compliance
Monitoring network compliance is vital for maintaining network adequacy standards. With Quest Enterprise Services, you can streamline this process, saving valuable time and reducing costs. Say goodbye to bulky compliance testing! Our innovative services allow you to allocate more resources to gain better insights into your data, analyze network performance, and take action where it matters most.
Build a Provider Network the Stands Out
Distinguishing yourself from the competition starts with building a provider network that meets the unique needs of your potential demographic and delivers exceptional care. With Quest Enterprise Services, gaining enriched data insights becomes effortless. Easily identify and recruit top-tier providers who align with your organization’s goals and preferences. Let us help you create a network that sets you apart and exceeds expectations.
Provider Network Modeling, Tracking & Trending
Understanding how network changes impact your network’s strength is crucial. That’s where Quest Enterprise Services comes in. Our platform equips you with tools to easily track network performance over time, giving you a clear view of any adjustments you make. Armed with these insights, you can confidently make informed decisions and tackle any challenges that come your way.
Dedicated Consultants for Expert Support
Choosing Quest Enterprise Services means having a team of expert consultants with deep industry knowledge ready to support you. Whether you’re starting or looking to grow, our Quest Analytics Consultants will be your guiding stars. You can focus on the big picture while we handle all the heavy lifting of data management, outreach, and analysis.
Quest Enterprise Services Exception Package for Network Adequacy Justification
Sometimes, your application may fall short of network adequacy standards. But don’t worry, our Quest Enterprise Services Exception Package is here to assist you. With our solution, we help you present a strong case and align with various regulatory requirements to streamline your network adequacy justifications.
Compliance with Provider Directory Accuracy Requirements
We’re not just about network adequacy requirements. Increasing provider directory accuracy requirements at federal and state levels introduces additional complexities that require your attention. Quest Enterprise Services Accuracy is designed to help you navigate the intricacies of the changing requirements and stay compliant. Learn how you can meet regulatory requirements and avoid those unwelcome surprises along the way!
QHP MARKETPLACE RESOURCES
Stay up-to-date on the latest network adequacy requirements and best practices for Qualified Health Plans (QHPs). Explore our growing library of blogs, briefs, videos and more!
Get Started with Quest Enterprise Services Today!
Contact us to schedule a demonstration and learn how Quest Enterprise Services can help you stay compliant, maximize efficiency, and achieve network adequacy with ease.