Provider Data Accuracy Resource Hub
Looking to improve your provider data accuracy and stay compliant with federal and state regulations? You’re in the right place! Dive into our growing resource library, packed with the latest news, actionable tips, and expert guidance to help you build a stronger, more reliable program.
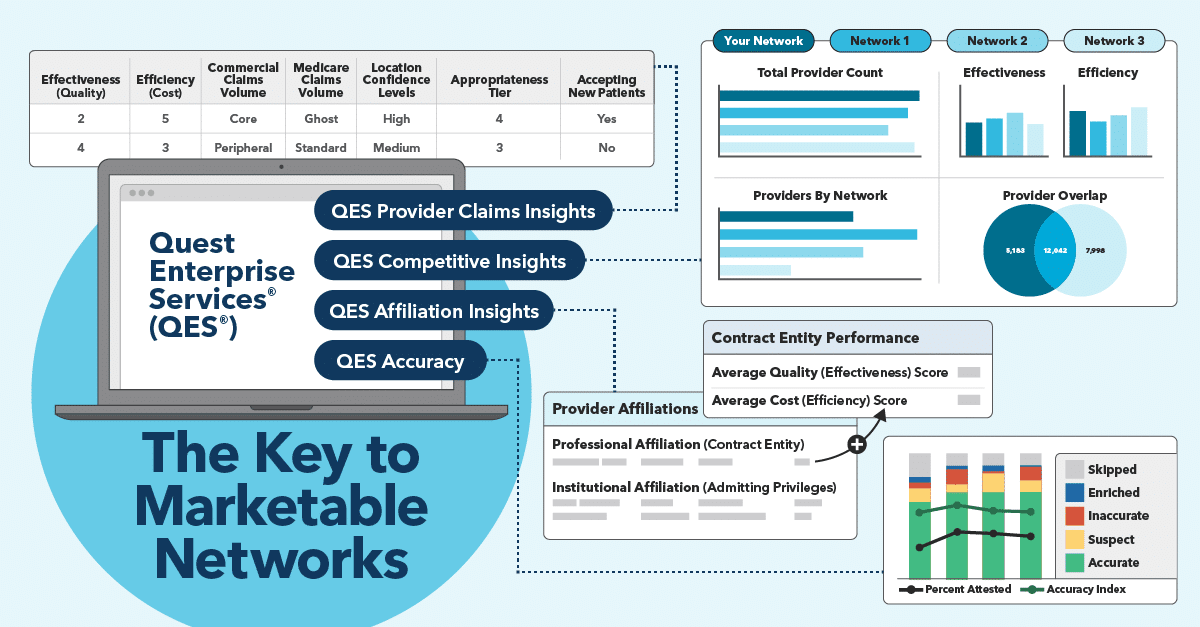
What if you could pinpoint where your provider network data stands and get the insights you need to succeed in your next directory audit? That’s what Vince Savickis, Solution Executive at Quest Analytics and his team, helped 10 health plans – who weren’t yet using Quest Analytics Accuracy Solution & Services – achieve.
Kate Deiters sits down with Vince to discuss the key findings, including the top three provider data errors, the evolving compliance requirements, and the practical steps to take to improve your data accuracy.
Featured Resources
No Surprises Act Resources
Ghost Networks Resources
Listen to Our Latest Podcast Episodes
Find More Videos from Quest Analytics
Learn the latest news, insights, and strategies, from the experts at Quest Analytics. Explore our collection of provider network management videos on our YouTube channel.
🔔 Subscribe Today to be the first to access new content as soon as it’s released!
Join a Webinar On-Demand
Provider Data Management Tips to Successfully Meet the No Surprises Act
Health plans must have a documented, defendable process in place to show the effort they’re making to comply with the provider directory verification requirements. What should this process look like? We have the answer!
FAQs and Provider Directory Requirements: Key Tips and Targets
We answer the most frequently asked question that health plans are asking us regarding the CAA Provider Directory Requirements. We also share tips and targets to help you get ahead in the coming months.
The Hottest Trends across health insurance markets
The data is in—and it’s clear: provider network oversight, provider data accuracy and provider data transparency are the hot trends across all health insurance markets. Find out what this means for you.
On-Demand Webinar: AHIP & Quest Analytics Present
STAY AHEAD OF NEW PROVIDER DIRECTORY REQUIREMENTS
Quest Analytics partnered with AHIP to continue the conversation about the new Provider Directory Verification requirements listed in the No Surprises Act. Watch now and learn about:
- The new provider directory accuracy requirements for health plans and providers
- The impact the requirements have on your business
- Which strategies to implement now
On-Demand Webinar
No Surprises Act: What You Need to Know and Why
The No Surprises Act includes regulations that will affect most of our health plan clients. As many are just learning about the new provider data requirements, we want to share the cliff notes and answer the most common questions. Watch the on-demand webinar to learn best practices, strategies, and actionable steps you can take today to align with the new federal requirements.
The New Provider Directory Accuracy Mandate
Under the No Surprises Act, commercial, qualified health plans (QHPs), and employer-based health plans are required to maintain accurate provider directories. Read our legislative brief to learn about the new requirements that health plans and providers need to meet.

White Paper
Surprises in the No Surprises Act for Health Plans and Providers
The new provider directory verification requirements continue to surprise most health plans and providers. Discover what each party needs to do to update the provider directory, and how to design your process to comply with the accuracy requirements.
Best Practices
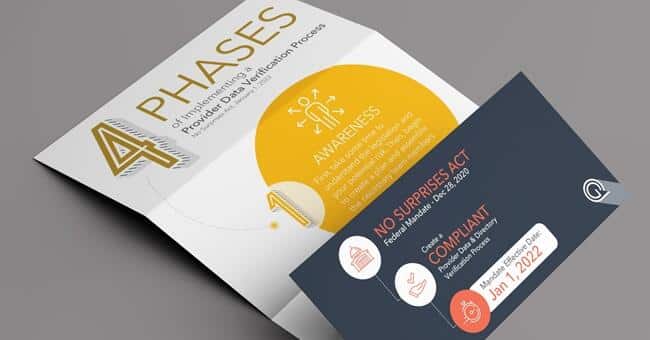
Implementation In Four Phases
There is a lot to consider and accomplish as you prepare for the mandate. Where do you begin? What happens next? What is a realistic timeline? We’ve mapped out the process for you. Download the Four Phases of Implementing a Provider Data Verification process.

Best Practices
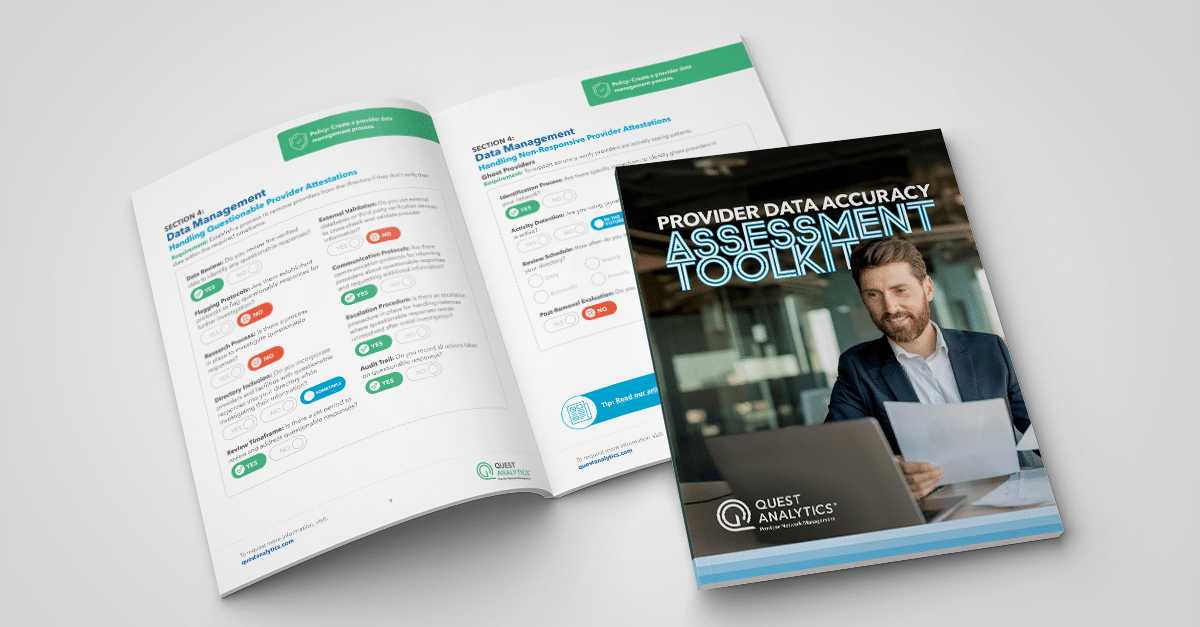
Eleven Questions to Ask Your Teams
As a best practice when preparing for the Provider Data and Directory Verification mandate, it is imperative that you understand your current process. Download the top eleven questions we recommend you ask your teams.
Best Practices
Frequently Asked Questions
Section 116: Protecting Patients and Improving the Accuracy of the Provider Directory Information, requires health plans and providers to work together to maintain up-to-date provider directories. Discover the answers to the top questions about the new requirements.
LEARN MORE WITH RELATED RESOURCES
Success Stories
Schedule Your Complimentary Strategy Session
Compliance isn’t our name, but it sure is our game! Learn how we can assist your efforts to make your provider data accurate and network adequate. Book a complimentary strategy session with a Quest Analytics expert to get started on your quest for success.