Facing the Realities of Provider Data Challenges to Improve Outcomes
About This Webinar
Data Integrity is foundational to provider networks, and with the evolving regulatory landscape generating increased scrutiny around the accuracy of provider directories, like the No Surprises Act, it’s more critical than ever to have tools, insights and processes in place to meet regulatory compliance while improving your outcomes, performance, and overall member experience.
While provider data is foundational to many processes, inaccurate provider data is a systemic issue – and from regulators to health plans to providers, everyone is trying to fix it. We’ll take a deep dive into real-world scenarios from three different perspectives (payer, regulatory, and industry) on tackling today’s provider data accuracy challenges – each with best practices and cautionary tales to share.
By watching this webinar, you’ll gain
- A better understanding of the regulatory risk of inaccurate provider data, and how to become more compliant confident
- Best Practices on how to simplify your accuracy review and processes to help streamline data improvements
- Proven tactics for creating operational efficiencies and reducing outreach efforts
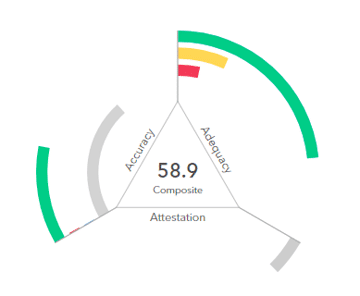
Gain a Clear Understanding of Quest Enterprise Services Accuracy
Dynamic, Transparent, and Proven Provider Data Accuracy Services
Experience the transformative power of dynamic, transparent, and proven provider data accuracy services. Download our overview to learn about our individualized and continual approach to provider outreach and attestation.
More Provider Data Accuracy Articles


5 Best Practices: Improving Provider Data Accuracy, Provider Outreach and Outcomes
Learn five best practices to improve your provider data accuracy, provider outreach, and provider data management processes.
How to Increase Practitioner Response Rates for Data Accuracy
Struggling to engage healthcare practitioners for data accuracy? Our proven strategies will increase response rates and simplify the process! Read our article to learn more.
Improve Verification Process & Data Accuracy with 90-Day Outreach
Optimize provider outreach and verification with Quest Analytics. Get a better understanding of our 90-day rolling approach.
Proven Solutions for Your Provider Network Management
Looking to simplify your workload? Let Quest Analytics take on the heavy lifting! Our solutions and dedicated team specialize in provider data accuracy and provider network adequacy for various lines of businesses, including Medicare Advantage, Medicaid and Commercial. Schedule a strategy session today and see how we can help you every step of the way.