On October 4, the Centers for Medicare & Medicaid Services (CMS) unveiled the proposed Notice of Benefit and Payment Parameters for the 2026 plan year (Proposed 2026 Payment Notice) alongside the 2026 Draft Letter to Issuers (2026 Draft Letter) in the Federally-facilitated Exchanges (FFEs). This significant release initiates the annual rulemaking cycle, shaping regulations for Marketplace plans and federal oversight of group and individual health insurance coverage. The proposed rule outlines several important provisions related to network adequacy, which will impact how qualified health plans (QHPs) and stand-alone dental plans (SADPs) are evaluated and managed.
Network Adequacy Overview
Continuing Policies in the Proposed 2026 Payment Notice and 2026 Draft Letter
For the 2026 plan year and beyond, CMS is rolling forward several established policies regarding QHP certification and network adequacy assessments.
Provider Network Requirements: QHPs must continue using a provider network, with an exception for SADPs.
Network Adequacy: Evaluated using time, distance, and appointment wait time standards.
Telehealth Services Reporting: QHPs must keep reporting telehealth services as they did the previous year.
Appointment Wait Time Standards: These will stay the same as in 2025, with health plans subjected to secret shopper surveys.
Coordination with State Authorities: CMS will keep working with state authorities to address network adequacy compliance, minimizing duplicate requirements and regulatory burdens.
💡 Want more information on the current requirements? Download our QHP policy brief.
Network Adequacy for Marketplace Qualified Health Plans
New Geographic Distance Methodology
While the time and distance standards remain unchanged from 2025, CMS proposes adopting a new methodology that uses geographic distance instead of estimated driving time. This method considers real-world conditions, such as terrains and infrastructures, which will help reduce the burden on issuers as CMS will be able to identify with greater precision the network gaps requiring attention.
New Way to Measure QHP Network Adequacy
Kate Deiters and Zach Snyder discuss the new Geographic Distance Methodology, which shifts away from relying solely on estimated driving time. Instead, this approach accounts for real-world factors such as the terrain, bodies of water, and infrastructure to give a better understanding of the landscape.
Dive Deeper with Our Full Podcast Episode! Get the full scoop on recent regulation changes and updates on network adequacy and provider directory accuracy. Listen Now
Essential Community Provider Certification Reviews in States Performing Plan Management
The Essential Community Provider (ECP) standards for the 2026 plan year will stay consistent with those set for 2024. However, starting with the 2026 plan year, CMS proposes to conduct ECP reviews for all FFE issuers, including FFE QHP issuers in States performing plan management functions.
States performing plan management functions include:
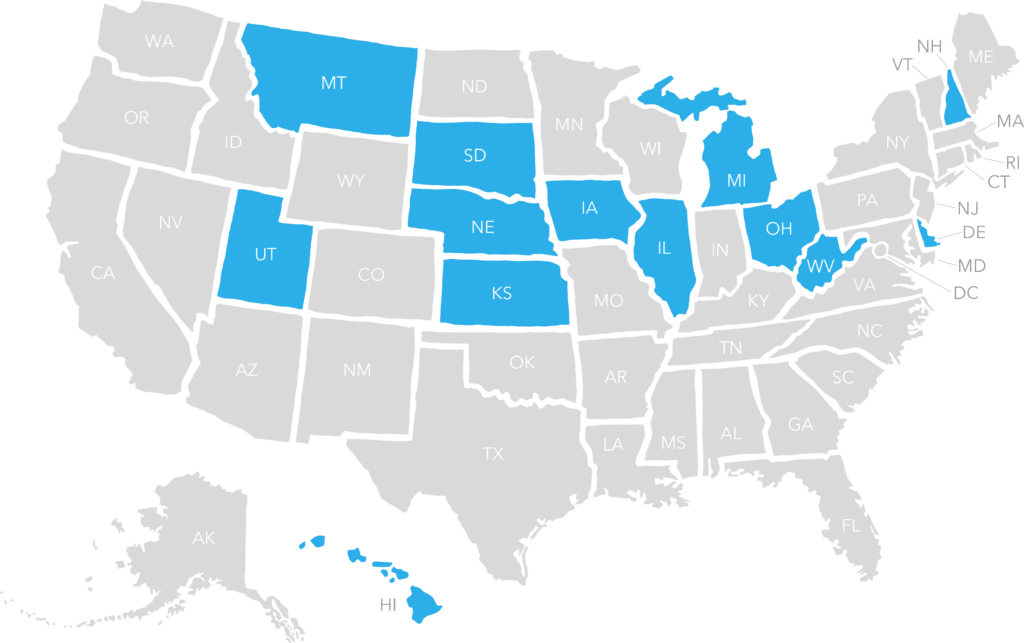
- Delaware
- Hawaii
- Illinois
- Iowa
- Kansas
- Michigan
- Montana
- Nebraska
- New Hampshire
- Ohio
- South Dakota
- Utah
- West Virgina
Request for the Reconsideration of Denial of Certification Specific to the FFEs
New Burden of Proof
CMS is proposing revisions to the request for reconsideration of denial of QHP certification, specifically for FFEs. If a health plan is denied certification, it will now need to provide clear and convincing evidence that CMS’ determination that the plan didn’t meet the certification criteria was an error. Essentially, the onus is on the health plan to submit a request to CMS for reconsideration of a denial determination and demonstrate that CMS clearly misunderstood or misinterpreted the facts or data already provided by the health plan in previously submitted application materials, for instance, network adequacy calculation errors.
Network Adequacy Justification Process
If a health plan doesn’t meet network adequacy standards, a satisfactory justification is required as part of their QHP certification application. The justification process remains unchanged from the 2025 plan year. Only the official Network Adequacy Justification Form, which is a partially prepopulated Excel document will be accepted by CMS. They’ll review updated provider data submitted on the issuer’s Network Adequacy Template and completed Network Adequacy Justification Form submitted as part of the certification process in assessing whether the issuer meets network adequacy before making the certification decision.
Note: Issuers should not use the Network Adequacy Justification Form to report their failure to contract with a third party to administer the secret shopper provider surveys.
💡 For more insights, download our QHP policy brief to learn more about the current process and requirements.
New Rules Explained! Get your guide to the updated QHP certification policies regarding network adequacy and provider data accuracy. Download the policy brief today!
Download Your Policy Brief
Quest Enterprise Services for QHP Issuers
In a market that never stands still, your strategy shouldn’t either. Backed by decades of industry leadership, Quest Enterprise Services® for Marketplaces and Exchanges offers your organization a proven approach to adapt and succeed in the Health Insurance Marketplace® and State Exchanges.
Industry-Leading Network Adequacy: At the core of Quest Enterprise Services® are our industry-leading network adequacy capabilities. Our offerings include the renowned CCIIO QHP FFE Network Adequacy Template and state-specific Exchange Network Adequacy templates that align with regulatory requirements.
Regulator-Approved Provider Directory Accuracy: Stay compliant with the No Surprises Act and state provider directory requirements. We simplify ongoing provider outreach, verification, and data dissemination.
With Quest Enterprise Services, you’ll not just participate, but lead in the Marketplace. Book a consultation with one of our Marketplace Experts to get started today.
More On Provider Data Accuracy and Network Adequacy
Proven Solutions for Your Provider Network Management
Looking to simplify your workload? Let Quest Analytics take on the heavy lifting! Our solutions and dedicated team specialize in provider data accuracy and provider network adequacy for various lines of businesses, including Medicare Advantage, Medicaid and Commercial. Schedule a strategy session today and see how we can help you every step of the way.