Compliance serves as a hallmark of integrity and a complex challenge for contemporary businesses. It’s an indispensable aspect of corporate governance that keeps companies in good standing with regulatory bodies and maintains their license to operate. For stakeholders in the healthcare sector, specifically those involved with Medicare Advantage plans, the Triennial Network Adequacy Review stands as a critical juncture in operational sustainability and regulatory compliance. This review plays a vital role in the longevity of healthcare plans, highlighting its significance in day-to-day operations and long-term strategic planning.
What is the Triennial Network Adequacy Review for Medicare Advantage Organizations?
The Triennial Network Adequacy Review is a comprehensive evaluation conducted every three years by the Centers for Medicare & Medicaid Services (CMS). It is integral to CMS’s routine oversight, checking whether a Medicare Advantage (MA) Organization’s provider network meets the standards for network adequacy and provider directory accuracy.
How are Plans Selected for the Triennial Network Adequacy Review?
Contracts for the Triennial Review are selected by CMS, based largely on the contract’s last full-network review. Although reviews are typically on a three-year cycle, certain events may trigger an earlier audit.
Triggering Events for a Triennial Review
CMS may perform a network review after triggering events such as:
- Initial Application or Service Area Expansion (SAE) Application; Applicants who use Letters of Intent (LOIs) to meet network adequacy standards during the application process are required to participate in the triennial review in the first year that the contract(s) are operational in the new service area.
- Significant Provider or Facility Contract Termination
- Complaints Regarding Network Access
- Organization-disclosed Network Gaps

Elevate your provider network with our free audit toolkit! Discover opportunities to stay compliant, enhance data management, and optimize network performance.
Free Provider Network Adequacy and Provider Data Accuracy Audit Toolkit
What is the Operational Process For a Triennial Network Adequacy Review Audit?
Timelines and Phases of the Audit Process
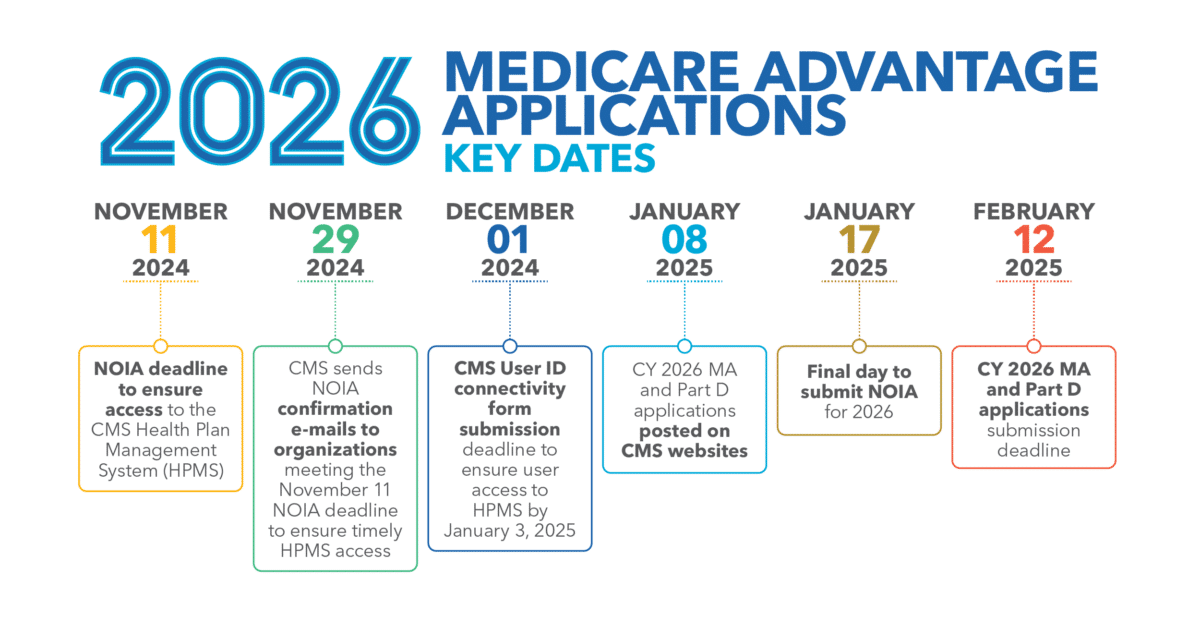
Audit Notification: MA organizations generally receive a notification in December regarding their selection for the upcoming review, scheduled to begin the following June. The notice includes detailed instructions for submitting the required network data and documentation.
Consultation Review: From January to May, MA organizations may participate in a non-binding Consultation with CMS. This is an opportunity for the MA organization to upload its network data in the Network Management Model (NMM) for an informal review and technical assistance.
Formal Submission: In mid-June, the submission of Healthcare Service Delivery (HSD) tables is due, which CMS reviews over the following months. During this phase, MA organizations will have the opportunity to submit network adequacy exceptions.
HSD Tables Submission Procedure
To demonstrate compliance, MA organizations must complete and submit two HSD tables—one Provider and one Facility HSD table—per contract for the CMS to evaluate. Each HSD table must include the required information and be submitted to the NMM in the Health Plan Management System (HPMS).
MA organizations submit two HSD tables for each contract:
- A Provider HSD Table
- A Facility HSD Table
What's Required for Provider Directories in the Triennial Network Adequacy Review?
Provider data accuracy is a crucial element of the triennial network adequacy review for MA organizations. To maintain compliance with federal mandates, HSD tables must match the provider directory. Additionally, MA organizations must reach out to providers to verify the accuracy of their listed information at least every 90 days.
Key data elements mandated for verification:
- Provider Name
- Provider Specialty
- Whether or Not the Provider Accepts New Patients
- Practice Address
- Phone Number
- Provider Offers Telehealth Services
- Provider’s Cultural and Linguistic Capabilities, Including Languages and American Sign Language
Updating Directory Information
When updates to provider details are received, MA organizations are responsible for updating their directories promptly. Any changes must be incorporated within 30 days of notification.
👉 Discover strategies to improve provider data accuracy and outreach methods in our article: 5 Best Practices: Improving Provider Data Accuracy, Provider Outreach, and Outcomes.
What is the Cost of Non-Compliance?
Should an MA plan fail to meet the standards during this review, it can face several compliance or enforcement actions, including Civil Monetary Penalties, intermediate sanctions like suspending marketing, enrollment, and payment processes, or in extreme cases, contract terminations.
Strategies for Maintaining a Thriving and Compliant Provider Network
Discover the best strategies for maintaining a thriving and compliant provider network with Eliza Hoffman, VP of Regional Payers at Quest Analytics.
How Can MA Organizations prepare for the Triennial Network Adequacy Review?
MA organizations can prepare by reviewing and updating their network data, ensuring they meet CMS’s current network adequacy standards, conducting internal audits, and addressing potential gaps in coverage or provider contracts well before the submission deadline.
- Leverage the Advance Notice: After receiving the December notification, gather, organize, and review all necessary documentation and data.
- Engage in the Consultation Phase: Participate in the informal review and seek technical assistance to rectify potential issues before the formal review.
- Prepare Documentation Thoroughly: Ensure all data, especially within the HSD tables, is accurate, complete, and meets CMS requirements.
Quest Analytics: Facilitating Compliance and Competitive Advantage
Successfully navigating the Triennial Network Adequacy Review is more than a compliance obligation; it’s a strategic advantage in the competitive healthcare market. By aligning with CMS requirements and ensuring a high-quality provider network, MA organizations can enhance their market standing.
For organizations striving to excel in the Medicare Advantage landscape, understanding triggering events, preparing meticulously for reviews, and maintaining continuous compliance through effective network management are key to transforming regulatory challenges into operational and strategic success opportunities. Engaging with partners like Quest Analytics can provide the technology and expertise needed to navigate the complexities of regulatory compliance, transforming the Network Adequacy Review from a challenge into a strategic asset.
Connect with one of our experts today to explore how we can convert regulatory challenges into opportunities for success in your Medicare Advantage strategy. Start a Conversation
More On Provider Data Accuracy and Network Adequacy
Proven Solutions for Your Provider Network Management
Looking to simplify your workload? Let Quest Analytics take on the heavy lifting! Our solutions and dedicated team specialize in provider data accuracy and provider network adequacy for various lines of businesses, including Medicare Advantage, Medicaid and Commercial. Schedule a strategy session today and see how we can help you every step of the way.