Health Systems & Provider Groups
Accelerating Success for Health Systems
Understand and Elevate the Value of your Health System’s Network
Navigating the complexities of a seamless care continuum – with the least amount of provider abrasion and patient leakage from your health system — can be daunting. It takes insight into referral patterns, utilization, physician performance, market awareness, and positive patient experience. Simultaneously, it’s crucial to maintain a delivery network that provides reasonable access to high-quality care across all specialties and that provider information is up to date and correct. We can help.
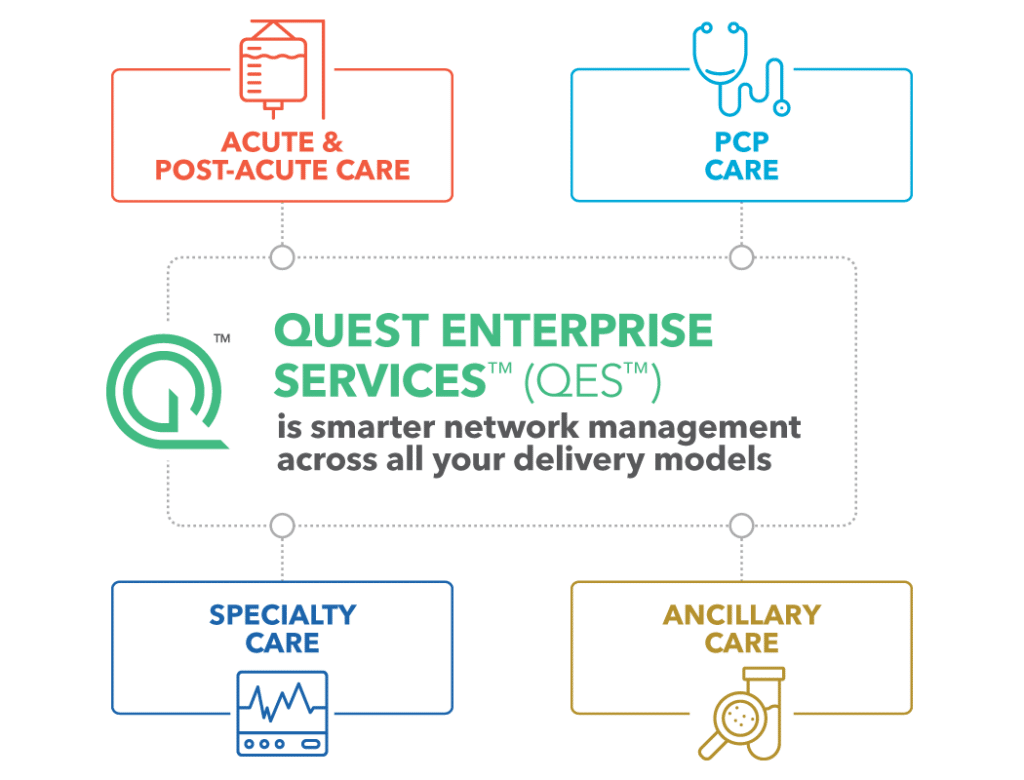
Quest Analytics helps you leverage information and insights into a competitive advantage. With Quest Enterprise Services® (QES®), you can build and optimize a clinically integrated network, quickly identify geographies where coverage is lacking, and then efficiently find high-performing, high-quality providers or medical groups to fill the gaps in care.
When you understand the value your network brings in terms of access, adequacy, cost and quality, and service locations, you help ensure better access to care (acute & post-acute care, specialty care, ancillary care, PCP care, etc.) for your patients while also improving your ability to negotiate with payer organizations.


Elevate Your Business Strategy
Evaluate your network using tools to examine top conditions treated and procedures provided by your specialists. This allows you to assess gaps in care and determine where to recruit providers to ensure you have comprehensive service offerings to keep your patients in your network.
Understand Your Network Performance
Leverage claims, cost, and quality information to understand the overall performance of your health system. Streamline your analysis of provider efficiency and effectiveness, review provider volume, identify ghost providers, assess specialty coverage, and gain valuable insights for risk-based contracts.
Strengthen Your Contract Negotiations
Empower your contract negotiators by providing them with compelling data that shows how your network alone can adequately support members of a payer network.
Elevate Your Business Strategy
Evaluate your network using tools to examine top conditions treated and procedures provided by your specialists. This allows you to assess gaps in care and determine where to recruit providers to ensure you have comprehensive service offerings to keep your patients in your network.
Understand Your Network Performance
Leverage claims, cost, and quality information to understand the overall performance of your health system. Streamline your analysis of provider efficiency and effectiveness, review provider volume, identify ghost providers, assess specialty coverage, and gain valuable insights for risk-based contracts.
Strengthen Your Contract Negotiations
Empower your contract negotiators by providing them with compelling data that shows how your network alone can adequately support members of a payer network.
Solutions to Support
At the heart of thriving healthcare practices is ensuring you have the providers, locations, and services needed to deliver high-quality patient care. Our Quest Enterprise Services® (QES® ), platform and supported solutions empower you with broad visibility into your provider network, enhancing your strategic and operational confidence. We equip you with the tools you need to understand your network’s value to payers and gaps within your network. This strategic insight not only strengthens your service delivery but also gives you a competitive edge during crucial payer negotiations.
Evaluate and curate your network to definitively demonstrate to payer partners or employee groups that your network provides access to care that their members require, meets or exceeds their cost and quality standards, and helps them ensure compliance with regulatory requirements.
Enhance provider data accuracy with our dynamic approach, featuring continuous and individualized outreach. Tailored strategies for small groups, individual providers, and large health systems allow you to optimize verification while gaining quick visibility into data changes and outreach metrics.
Leverage Provider Claims Insights (PCI) to evaluate service line access and performance, inform value-based pricing models, demonstrate cost-to-value ratios, and eliminate ghost providers for quality care in shared savings programs and employee plans.
Understand if you have the right providers at the right locations to adequately serve employee groups, a specific population, or the community at large. Analyze potential gaps in care across all specialties at a zip code level and fill any gaps with high-performing providers.
Negotiate from a position of strength by understanding the value of your health systems’ network within a larger payer’s network across several key dimensions for the payer: Network Adequacy, Cost and Quality, and Market Share.
The executive-level dashboard offers multi-level views of the strengths and weaknesses of your provider networks. Gain insights by geography or service lines, and easily drill down to areas of concern for detailed, micro-level analysis.
BETTERDOCTOR® FOR LARGE GROUPS & HEALTH SYSTEMS
SKIP THE PORTAL. SEND A ROSTER.
“With the tools I have from Quest Analytics, we take an offensive strategy with payers. We can tell them, ‘We are adequate. We can be in your network in a particular area without any other providers because we have everything covered from a CMS Medicare Advantage Network Adequacy regulatory perspective.”
— Sr. Network Development Executive, National Health System
“The Quest Enterprise Services Market Provider List is an amazing feature. It narrows down to the providers that are going to give you the largest gain toward network adequacy based on the specialty. Had we not had that feature, we would have spent more of our time looking at providers that wouldn’t have made an impact on what we needed. The ability to target those specific providers is so incredibly efficient.”
— Business Analyst, Regional Health Maintenance Organization
“I use Quest Enterprise Services almost every single day. I love the tools and can't wait for future enhancements.”
— Director of Network Data Analytics and Reporting, National Health System
“CMS requires valid addresses for the providers — and Quest Analytics made it very easy to identify those that we needed to fix.”
— Business Analyst, Regional Health Maintenance Organization
Discover More
Dive into additional resources for more information and valuable insights.
Get Started Today
Transform your provider network management with solutions that drive efficiency, compliance, and quality. Contact us today to learn how we can help you achieve your goals and excel in the ever-changing healthcare landscape.