CMS Medicare Advantage and Medicaid Resource Hub
Discover the latest insights and proven provider data management tips for CMS compliance. Our expanding collection of resources is here to help you achieve your Medicare Advantage Plan goals.
The REAL Health Providers Act has been signed into law, introducing new provider directory accuracy requirements for Medicare Advantage Organizations. These include a 90-day verification timeline, annual accuracy analyses, public directory accuracy scores, and more.
Latest Medicare Advantage News & Insights
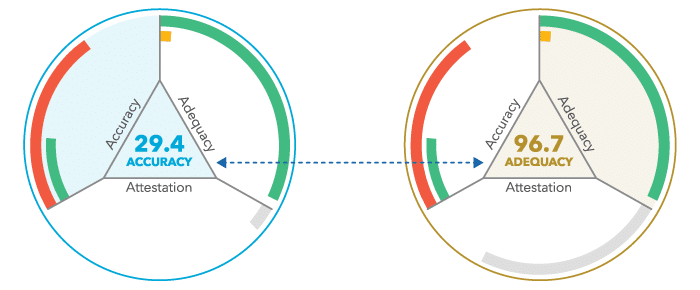
What if you could pinpoint where your provider network data stands and get the insights you need to succeed in your next directory audit? That’s what Vince Savickis, Solution Executive at Quest Analytics and his team, helped 10 health plans – that weren’t yet using Quest Analytics Accuracy Solution & Services – achieve.
Kate Deiters sits down with Vince to discuss the key findings, including the top three provider data errors, the evolving compliance requirements, and the practical steps to take to improve your data accuracy.
What to Do When Your Medicare Advantage Contract is in Jeopardy
Discovering network deficiencies after submitting your HSD table to CMS can be stressful. Where should you start if you want to quickly add providers to the network? Eliza Hoffman, our VP of Regional Payers Segment, shares the answer.
Network Adequacy Exception Resources
Ghost Networks
Join A Webinar
Find More Videos from Quest Analytics
Learn the latest news, insights, and strategies, from the experts at Quest Analytics. Explore our collection of provider network management videos on our YouTube channel.
🔔 Subscribe Today to be the first to access new content as soon as it’s released!
Success Stories
Measure Your Provider Network Like CMS
Ready to evaluate your provider network the same way that regulators will evaluate it? Quest Analytics delivers the answers to your test – bringing peace of mind by showing you what regulators will see when they evaluate your network. Our Medicare Advantage Network Adequacy templates will reduce your compliance testing time and cost, leaving you with more time to focus on getting better insight into your data and taking action where it matters.
Press Release
CMS Extends Its Contract With Quest Analytics
The Centers for Medicare & Medicaid Services (CMS) has extended their contract with Quest Analytics for an additional five-year term to measure the adequacy of all Medicare Advantage Part C & D and Medicare-Medicaid Health Plans’ (MMP) provider, facility and pharmacy networks.
Schedule Your Complimentary Network Assessment Today!
Interested in discovering how we can assist you with your service area expansion and network adequacy goals? Schedule your complimentary network assessment with a Quest Analytics expert today.