BRING NETWORK ADEQUACY TO YOUR ENTIRE ORGANIZATION
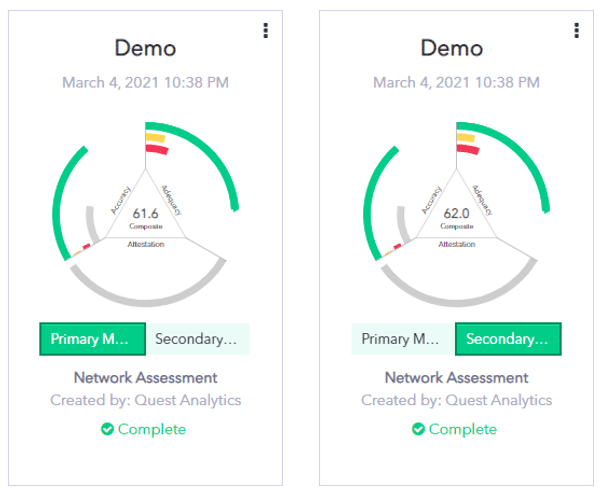
Quest Enterprise ServicesTM (QESTM) Adequacy solution provides your organization with the tools you need to easily measure, manage, and monitor network adequacy and network performance. Your team can see the status of all lines of business. With this type of visibility, you will be able to enhance cross-team communication, increase network transparency, streamline compliance monitoring processes, and have the information you need to differentiate your network. You are able to go beyond adequate standards to create excellent member experiences and a more competitive network overall.
MEDICARE ADVANTAGE NETWORK ADEQUACY
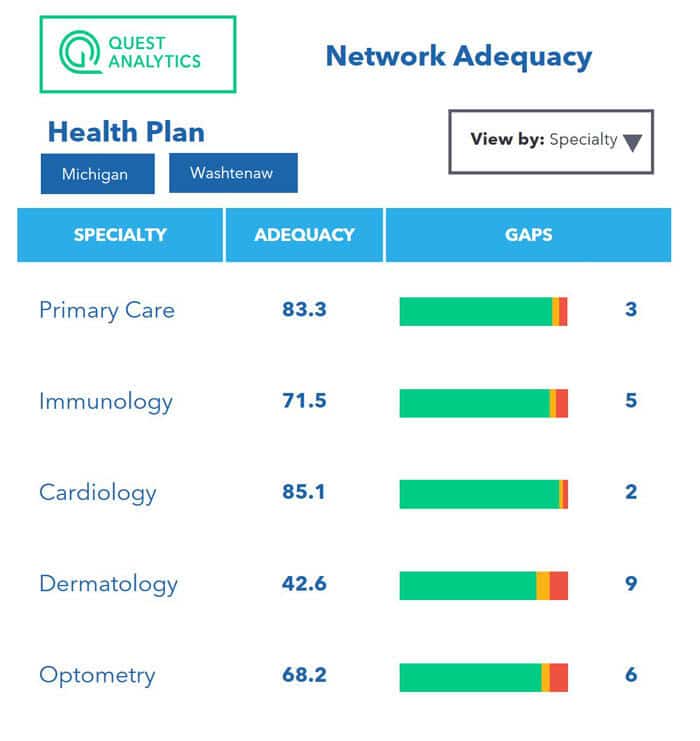
At the core of our Network Adequacy Services are the time and distance requirements, used by the Centers for Medicare & Medicaid (CMS). We then take the standard Adequacy Analysis to the next level by incorporating aggregate scoring, network trending, time-sliced comparisons, provider data management and identified changed providers. These additional insights give you a complete picture of your network.
You’ll find our executive summary dashboard is an invaluable tool for providing an overview of all the networks you manage. QES includes an aggregate adequacy score and allows modeling of your network to demonstrate what happens when providers are added and removed over time. This modeling includes insight into the impact removing inaccurate data will have on your network adequacy through our Accuracy Gap Analysis. This before and after view includes the number of additional gaps, the impact on your adequacy score and what inaccurate information caused the gaps.
Take your network analysis one step further and compare your network against current market providers to understand the depth of your network. View the gaps in your network, their age, and how they have changed daily, weekly or monthly.
Stay Compliant-Confident Year-Round
NETWORK ADEQUACY TEMPLATES
Streamline your provider network management for federal and state programs with our pre-built network adequacy templates. You can choose from templates aligned with the current Federal network adequacy standards & requirements for Medicare Advantage, Medicare-Medicaid, and Qualified Health Plans certification to participate in the Federally-facilitated Marketplaces (FFMs), as well as, an ever-growing list of state programs. See which templates are available for you today!
CCIIO QHP FFE Network Adequacy Template
QHP CERTIFICATION
Are you a Qualified Health Plan (QHP) on the Federally-facilitated Exchange (FFE) looking for a way to easily monitor the compliance of your provider network? If so, Quest Enterprise Services can help. We have a pre-built CCIIO QHP Network Adequacy template based on the latest CCIIO FFE QHP Network Adequacy requirements. Learn how our template helps you save time and stay compliant. QES CCIIO FFE Template
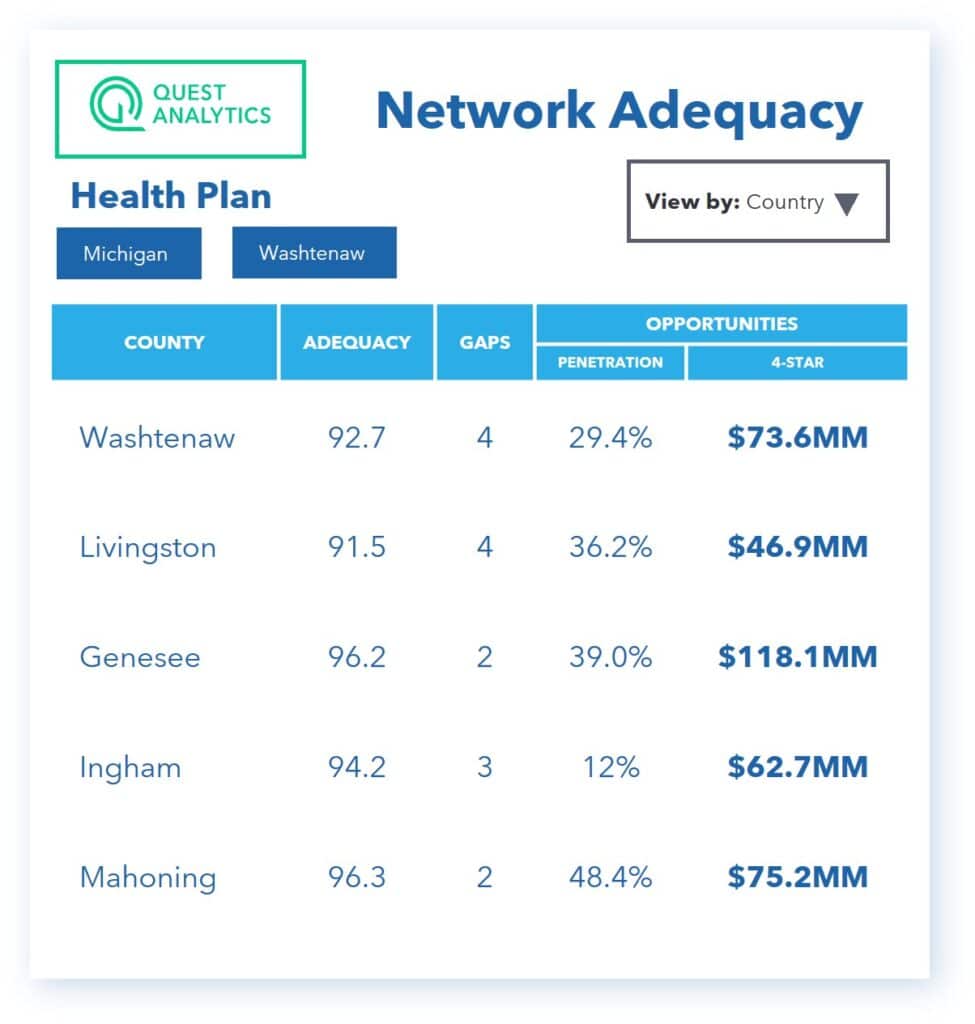
STREAMLINE YOUR SERVICE AREA EXPANSION EFFORTS
We get it – expansion efforts generally take a mountain of research and Herculean efforts to come to fruition. With the Adequacy solution, you can easily project and validate the next best counties to expand your plan. It can show you exactly how the expansion will affect your overall network adequacy and the effort that it will take.
The QES Adequacy solution provides you with smart recruiting, saving you time and resources. Easily run what-if scenarios to project adequacy when you target providers from your network data and market data. And discover providers who can fill adequacy gaps across your networks. Start optimizing your expansion plans by contacting us for more information.
Identify Ghost Providers
Identify ghost providers and optimize the value of your network, by ensuring it’s adequate, accurate, and active with Quest Enterprise Services Provider Claims Insights.
DRIVE WORKFLOW EFFICIENCY IN QES ADEQUACY
Accelerate your processes for managing your Medicare Advantage, Commercial, or Medicaid provider networks with our enhanced toolset. The time-saving features allow you to streamline processes for creating differentiated networks, gaining competitive advantages, meeting regulations, and achieving your business goals.
NETWORK ADEQUACY EXCEPTIONS
Wishing you could expedite the research part of the exception request process? It’s now possible! The Exceptions Package is designed to save you valuable time and simplify finding the facts that support your exception requests to regulators.
- Zip Code Summaries – Identify at a zip code level those members who do not have access to care within the regulatory standard.
- Next Closest Network Provider – Identify the distance and/or time to the next closest network provider. You can identify non-contracted providers as well as prospect or market providers too!
- Next Closest Market or Prospect Provider – Identify the next closest Market or Prospect Provider between members that do not have access and the Next Closest Network Provider within the established standard to provide for exception requests.
- Sources – Use the populated list within QES to easily select your sources from a drop-down list and then export it for the required form.
Dual Membership Analysis
Visualizing your provider network based on a federal or state provided beneficiary or census file is important to measure your network adequacy for compliance. You also want to see how much coverage your have for your members. Often, it is necessary to utilize your membership file or multiple membership files. Quest Enterprise Services allows you to upload your membership file and run comparative analyses.
- Membership Analysis – Run analyses based on your custom membership distribution file.
- Membership Compare – Compare analyses across membership distribution data or with the sample beneficiary file.
- Membership Risk – See the number of members at risk due to any deficiencies, or gaps, in your provider network at the state and county levels.
- Membership Binding – Assign a specific subset of your membership to a given specialty.
Volume Actions for
Provider Network Modeling
Managing large groups of providers or facilities individually can be a tedious and inefficient task, particularly when it stretches across multiple business lines. But what if there was a better way?
QES Volume Actions introduces the innovative option of ‘what-if’ scenarios, enabling you to evaluate the effects of targeting or terminating numerous providers and facilities. You can quickly understand the potential impacts and adjust your strategies for optimum outcomes.
Volume Reporting simplifies generating provider network reports. This enhanced efficiency, combined with the valuable insights gained from these reports, facilitates the development of more effective strategies.
Discover how QES Volume Actions can transform your network management process.

MEDICARE ADVANTAGE NETWORKS
CMS Network Adequacy Compliance 365 days of the year. Providing you a better way to maintain compliance for current and future networks.

COMMERCIAL NETWORKS
Helping you create competitive advantages in the marketplace. Plus, measure your network for URAC and NCQA network adequacy accreditation.
DENTAL NETWORKS
Deliver supreme products by accelerating your network management, providing transparency to partners and brokers, and staying compliant.

MORE THAN MEETS THE ROI
Case study – For Dee Bellanti at HealthNow New York Inc., smarter provider network management was a better investment than they imagined. This case study explores how a costly CMS penalty proved managing their provider networks the same old way simply wasn’t good business.