Quest Enterprise Services® (QES®)
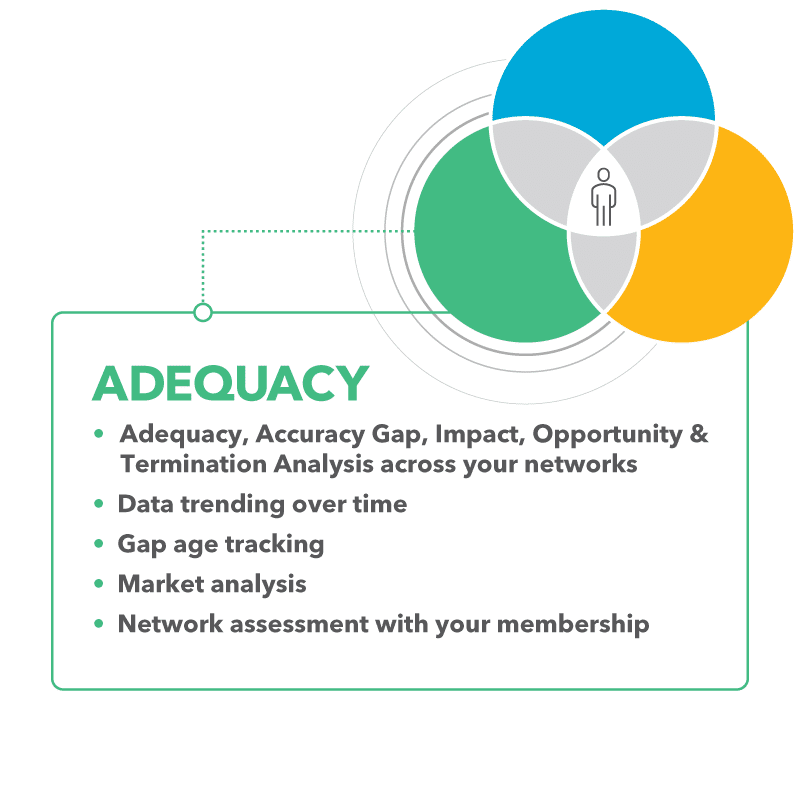
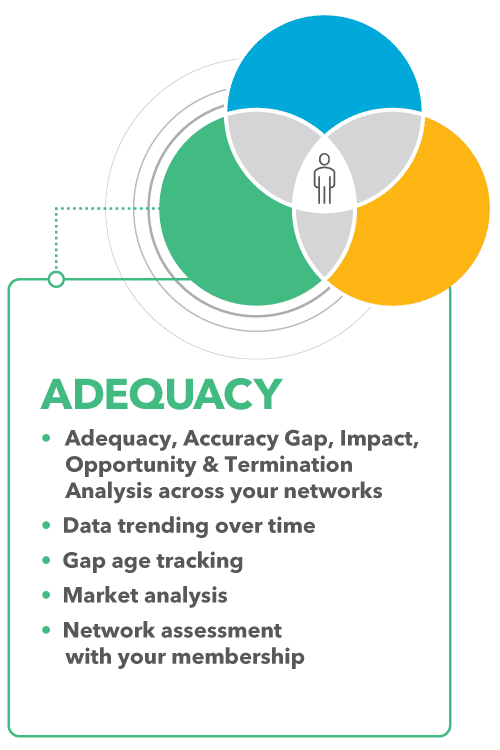
QES Adequacy
Industry Leading Network Adequacy Solution

Your Comprehensive Solution for Network Adequacy Compliance Management
Quest Enterprise Services® (QES®) Adequacy transcends traditional network compliance solutions, emerging as a pivotal asset for business growth and expansion. Tailored to effortlessly measure, manage, monitor, and model network adequacy and performance, QES Adequacy delivers value across all lines of business.
With enhanced data insights, visibility, and reporting, your team can streamline compliance processes, better understand the status of your network, improve collaboration, and make informed, data-driven decisions enterprise-wide. Your organization will be well-positioned to achieve its goals, capitalize on market opportunities, and confidently drive business forward.
Network Adequacy Compliance
Maintain network adequacy and adhere to regulatory requirements—relying on the same data and tools regulators depend on.
Improved Member Experience
Retain and grow your member population by ensuring your members have the right access to care, when and where they need it.
Network Management Efficiency
Build and expand your networks with adequacy analysis and insights that allow you to optimize operations in existing markets and leverage your current network to meet adequacy in new markets.
Proven ROI
Boost efficiency while capitalizing on new market opportunities with a single enterprise-wide platform.
- Popular Features
- Use Cases
- Related Solutions
- Related Resources
Popular Features
Explore the top features of QES® Adequacy, your keys to managing networks with precision across all lines of business, streamlining organizational efficiency, ensuring better member access, and minimizing network adequacy regulatory risks.
Network Adequacy Templates
Ensure compliance with regulator-endorsed Network Adequacy Templates. Access a robust collection of ready-made and customizable federal and state templates, featuring time and distance calculations, as well as county and zip code analysis.
Gap Management, Trending and Resolution
Increase visibility into network adequacy gap trends, identify specialties with compliance issues, and monitor the status of gaps and the time needed for resolution. With this insight, you can proactively address network gaps.
Provider Recruitment Tracking
Pinpoint providers to recruit to fill gaps, and track recruitment efforts throughout the year, streamlining your adequacy compliance efforts while supporting exception or justification requests.
Provider Impact Analysis
Gain valuable insights into provider availability within the market, across different lines of business, and the impact on your network adequacy based on geographic location and specialty.
Exception Management
Manage all network adequacy exceptions from a single solution. Gain the ability to create, update, track, and archive exceptions along with supporting documentation across multiple networks and lines of business.
Location Visualization
Improve network coverage and compliance reporting by using geographic visualizations to identify gaps in the network. These visualizations can include network coverage maps to pinpoint areas with low or no access and gap density maps to illustrate gap status geographically.
Compliance Monitoring
Streamline, measure, and monitor network adequacy scores across lines of business. Easily understand the source of compliance issues and the capacity of market providers to resolve it with color-coded highlights at the specialty and geography level.
Provider Network Adequacy Analysis
Identify whether your network has a sufficient number and type of servicing providers based on QES analysis that calculates and assesses time, distance, and provider ratio requirements across five different geographic county classifications.
QES® Adequacy in Action
QES Adequacy empowers health plans, ancillary plans, health systems, and regulators throughout the network lifecycle, helping them deliver the provider networks promised to consumers.
Payer Networks: Network Management Across Lines of Business
Take charge of network management across all lines of business, including Medicare Advantage, Medicaid, Marketplace, and Commercial. Gain a competitive edge by evaluating, managing, and reporting on provider network adequacy and provider data accuracy in a single platform—streamlined and scalable across your entire organization.
Health Systems: Gain Data Visibility and Strengthen Provider Networks
Operate with complete visibility into your participation, access, and adequacy across all payers in all service areas. Leverage your information and insights to gain a competitive advantage, particularly during contract negotiations with existing and prospective payer organizations.
Ancillary Plans: Increase Data Transparency & Streamline Compliance
Strengthen plan partnerships, secure government program contracts, and expand market presence with superior network management. Improve data transparency and cross-team collaboration, while maintaining compliance.
Regulators: Drive Innovation and Accountability in Healthcare Networks
Take an active role in transforming healthcare with the right network adequacy standards, improving provider directory accuracy, and ensuring compliance with health plan requirements. Equipped with reliable solutions and data insights, you can enhance oversight processes, promote transparency, and safeguard consumer protections—creating a more equitable and accountable healthcare industry.
Related Solutions
Strengthen your provider network at every stage by combining QES® Adequacy with additional tools. Gain actionable insights, increase operational efficiency, and build stronger networks. By integrating these tools, you’ll simplify workflows, reduce risk, and make more informed decisions—ensuring your healthcare networks excel at every stage of the lifecycle.
QES Accuracy
Leverage a continuously updated database of provider information as a reference file against your network information, supporting your network adequacy and performance efforts and outcomes.
QES Enterprise Compliance Dashboard
Leverage executive-level dashboards that provide network adequacy insights across your lines of business and networks, allowing leadership and teams to make strategic decisions focused on network adequacy.
QES Exceptions Package
Enhance Network Adequacy Exception Request process with exception narratives and expedite reports by using zip code summaries and the next closest provider allowing you to save time and help regulators better understand the justification for the network adequacy exception.
QES Membership Package
Model and assess your network using your member data and membership measured by regulators. You can also prioritize filling deficiencies based on the amount of membership at risk.
QES Provider Claims Insights
Improve your network performance with claims data, including volume of claims, payer mix, cost, and quality, as well as top procedures and conditions embedded into the QES platform to help eliminate ghosts, select the best provider to fill network gaps, and assist with expansion efforts.
QES Scenario Modeling Package
Simplify large-scale provider network analysis and reporting with three powerful tools. Create value-based or tiered networks with better modeling while improving your strategic understanding of how current and future provider contracts impact your network adequacy.

Discover More
Dive into additional resources for more information and valuable insights.
DELIVER ON TOMORROW’S GOALS BY PLANNING TODAY
Elevate your network management strategy today with Quest Enterprise Services® (QES®) Adequacy. Transform compliance tasks into growth opportunities and drive your business forward with confidence.
Schedule a complimentary consultation with one of our experts today to learn more.

Start a Conversation Today!