Consideration for Health Equity Measures in Network Adequacy Standards

The Affordable Care Act (ACA) directed the Centers for Medicare & Medicaid Services (CMS) to establish rules to require that Exchange health plans ensure a sufficient choice of providers.1 To implement this requirement, CMS adopted quantitative standards, which require Exchange health plans to ensure that its network providers are available to members within specified time and […]
Improving Network Adequacy and Access For Mental Health

Federal and state policymakers are taking a variety of measures to improve access to mental health services and substance use disorder treatments. Network adequacy and access are prominent areas of such a response directly affecting health plans. This blog post informs stakeholders about the increased emphasis on behavioral health networks and tips on how to […]
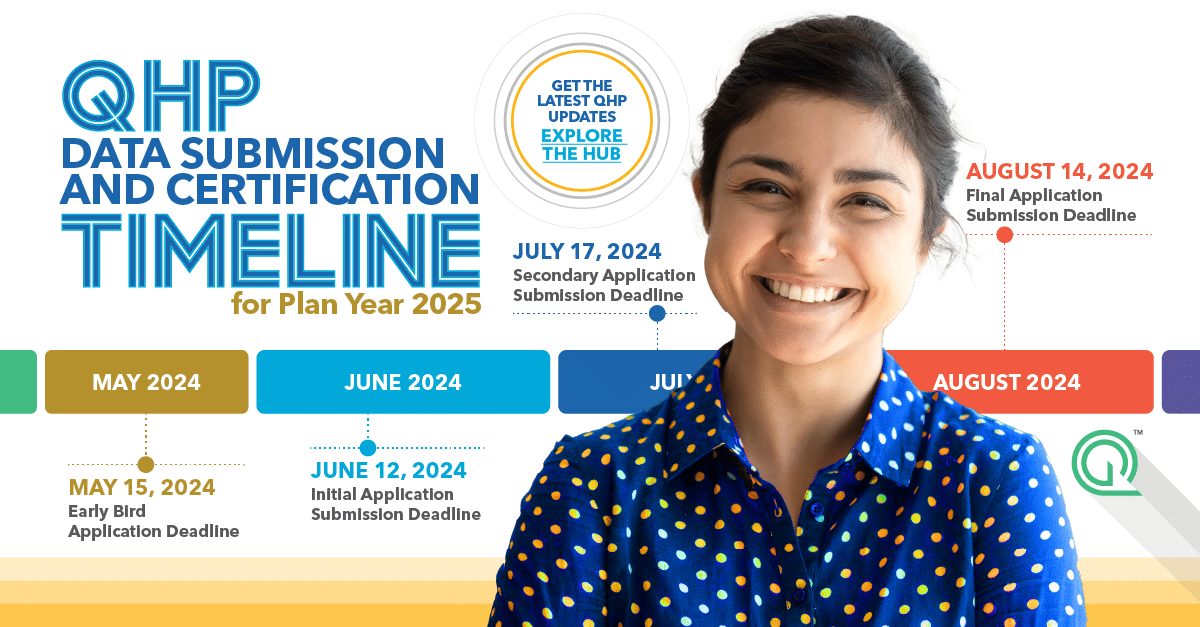
Key Application Dates: Unpacking The CMS Medicare Advantage Calendar
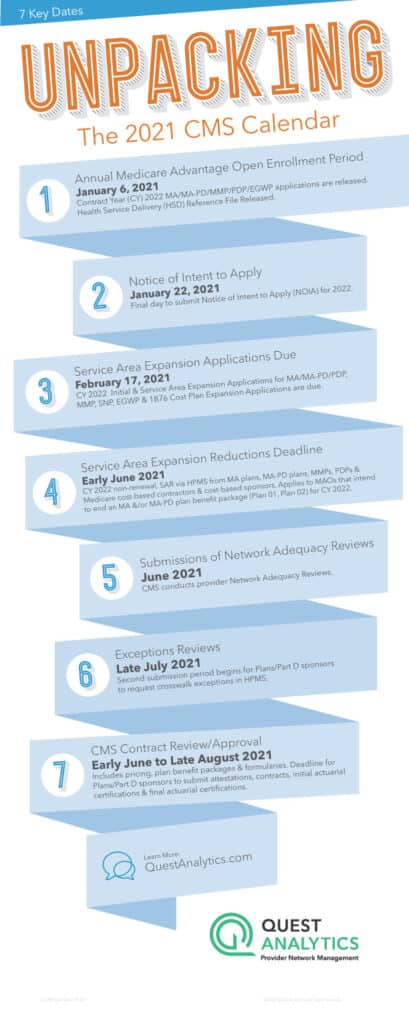
Centers of Medicare & Medicaid Services (CMS) Key Application Dates for CY 2022 Medicare Parts C and D Annual Calendar Our CMS calendar is one of the easiest ways to stay up-to-date with important dates and timelines for CY 2022 Medicare Advantage (MA) plans, Medicare Advantage-Prescription Drug (MA-PD) plans, Prescription Drug Plans (PDPs), Medicare-Medicaid Plans […]
Top 3 Things the “No Surprises Act” Means for Health Plans

It’s staggering to think that, according to researchers, one in five emergency room visits result in an individual receiving a bill for treatment or services they expected to be covered by their health plan, but weren’t. These unexpected, costly, and often frustrating charges are aptly called Surprise Medical Bills. While surprise medical bills impact consumers financially, […]
Designing and Building Clinician Networks That Address Social Determinants of Health
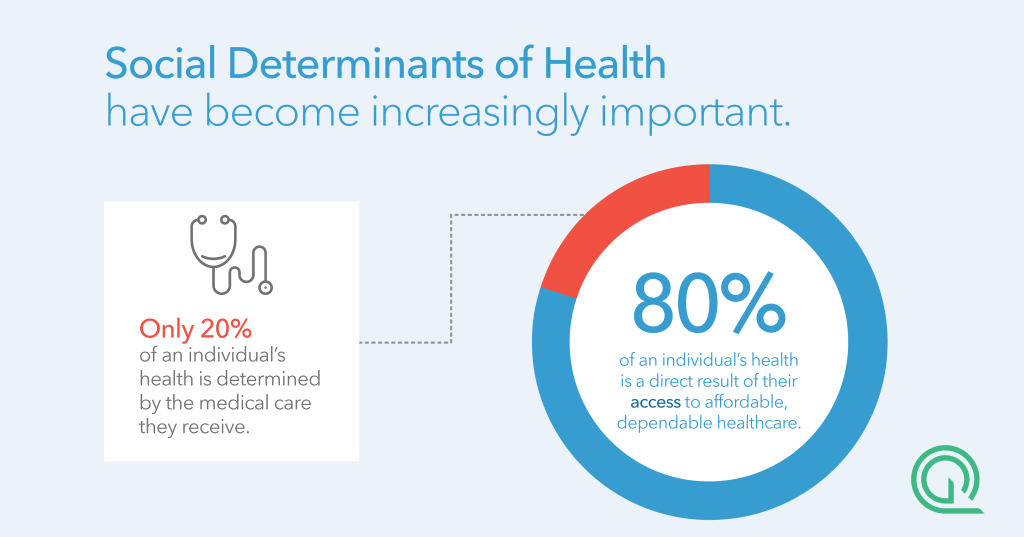
FIVE TAKEAWAYS FROM OUR WEBINAR Watch: Designing and Building Clinician Networks That Address Social Determinants of Health As clinicians and payers take on increasing risk for patient outcomes, it is essential that leaders consider the effectiveness of their networks as well as the accuracy of their clinician directories to ensure they are adequately serving their members. Modern […]
5 Things I Learned at Vision Quest

Admittedly, I’m new to provider network management. I’ve spent years working in healthcare, but this is my first time working with payers from across the nation to improve the access, adequacy, and accuracy of their provider networks. Lucky for me, I got a behind-the-scenes view through Quest Analytics Vision Quest. As a session moderator, I heard […]
New Metrics are Critical to Addressing Mental Health Access Concerns
Our new normal is far from normal. There is this level of incredible, nonstop uncertainty around our current situation, and none of us are immune. CDC data, collected in late June, noted an increase month-over-month in mental health issues. It showed that 40 percent of adults struggled with anxiety, depression, suicidal thoughts and substance abuse1. […]
The Rebirth of Network Adequacy: Modernizing Health Plan Practice

Reprinted from The URAC Report. Nearly two months ago now CMS finalized changes to Medicare Advantage (MA) and Part D for 2021 and while I previously covered the new telehealth network adequacy provisions, I’ve been meaning to do a deeper dive into how network adequacy as a whole has changed in recent years. To do this, I reached out to Cari […]
Preparing for the Era of Provider Network Transparency

Copyright 2020 Compliance Today, a publication of the Health Care Compliance Association (HCCA). Transparency is one of the top buzzwords in healthcare today. In the last few years, we have seen the rollout of significant healthcare transparency initiatives focused on portable health records, hospital costs, drug costs, quality data, and many other things (e.g., Executive […]
Rule Raises Questions About Telehealth, Directory Accuracy

Reprinted with AIS Health permission from the July 2, 2020, issue of RADAR on Medicare Advantage. As Medicare Advantage and other insurers report increasing use of telehealth during the COVID-19 pandemic and consider the larger role that virtual visits could play on a more permanent basis, CMS recently finalized a set of policies for 2021 […]