TAKE CHARGE OF YOUR PROVIDER NETWORK MANAGEMENT CHALLENGES
Welcome to a space designed for federal and state regulators, insurance commissioners, and health policymakers at all levels to drive conversations around ensuring timely and appropriate access to care.

DEVELOPING The FRAMEWORK FOR TELEHEALTH CREDITS AND NETWORK ADEQUACY STANDARDS
Considerations for Health Policymakers and Regulators
Telehealth services have transformed healthcare delivery. In response, health plan regulators have incorporated telehealth credits into health plan network adequacy standards. While this was a positive step, using a blanket approach to applying these credits toward network adequacy standards may not be the ultimate solution.
Our white paper provides insights into on how policymakers and regulators can address the challenges of incorporating telehealth credits into network adequacy standards.
NETWORK ADEQUACY AND HEALTH EQUITY
On his first day in office, President Biden signed Executive Order 13985, Advancing Racial Equity and Support for Underserved Communities Through the Federal Government.
Established a government-wide initiative to advance diversity, equity, inclusion, and accessibility.

CMS REQUEST FOR INFORMATION ON STRENGTHENING MEDICARE ADVANTAGE
The Centers for Medicare & Medicaid Services (CMS) released a Request for Information (RFI) seeking feedback on how to strengthen the Medicare Advantage (MA) program in ways that align with the Vision for Medicare and the CMS strategic pillars.
NETWORK ADEQUACY:
Shaping the Future of Healthcare
As a health plan regulator, you’re tasked with ensuring that consumers have access to high-quality, affordable coverage that meets their needs. What’s more? You need to be able to demonstrate sound policy and fiduciary oversight of health plans. That’s a lot to keep up with. And we’re here to help.
Over the past 15 years, we have been the trusted partner to the Centers of Medicare & Medicaid Services and more than 20 state regulators who oversee provider network adequacy for insurers. Regulators use our solutions, services and expertise to drive the evolution of network adequacy standards, improve provider directory accuracy, monitor compliance with health plan requirements, and provide transparency and consumer protections in the marketplace.
We are continually collaborating with federal policymakers, State Insurance Commissioners and State Medicaid Directors, helping them develop strong oversight of health plans to ensure they meet all federal and state regulatory requirements. We welcome the opportunity to meet with you and discuss how we can further support your efforts to improve access to care.

Press Release:
CMS EXTENDS ITS CONTRACT WITH QUEST ANALYTICS
MEDICAID

FEDERAL MEDICAID NETWORK ADEQUACY STANDARDS
Quest Analytics stands by to partner with State Medicaid Agencies to help develop quantitative network adequacy standards that are compliant with federal standards outlined in this brief. Given Quest Analytics’ knowledge of evidence-based quantitative network adequacy standards, our strong relationships with network adequacy leaders inside the Centers for Medicare & Medicaid Services, and our contractual relationships with Managed Care Organizations, Quest Analytics is in a strong position to offer expert assistance to any State in the development of standards.
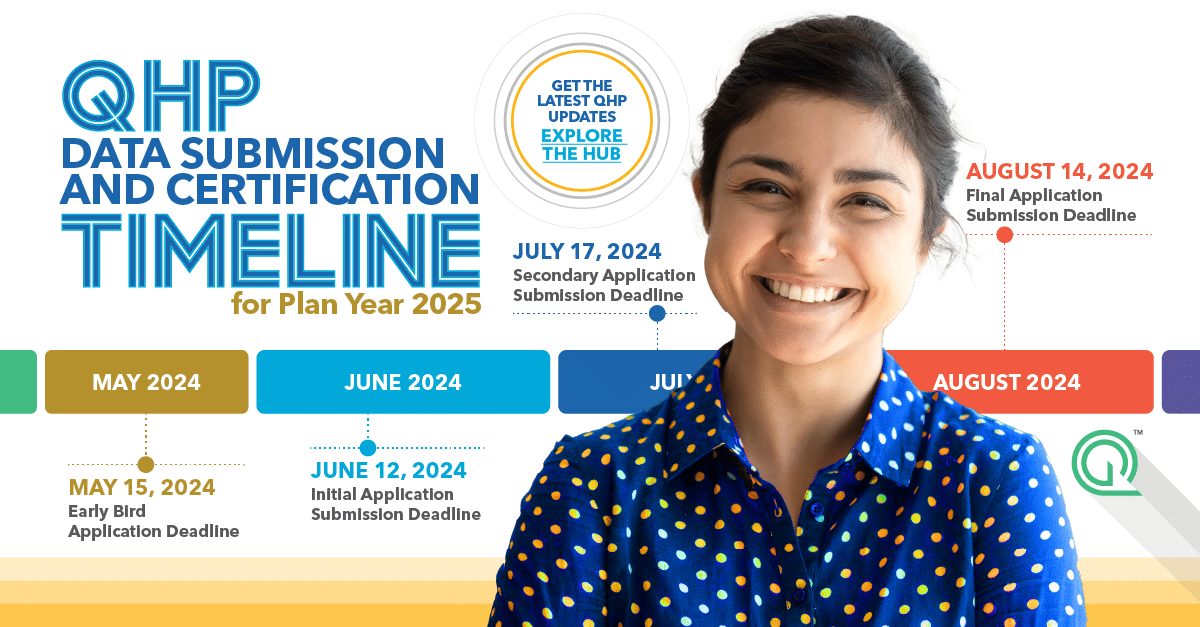
THE MARKETPLACE

Quest Analytics Comments on the Notice of Benefit and Payment Parameters for 2023
INCORPORATE HEALTH EQUITY MEASURES INTO EXISTING NETWORK ADEQUACY STANDARDS
In January 2022, we submitted a comment letter to the Center for Medicare & Medicaid Services (CMS) on the agency’s request for feedback related to advancing Health Equity in Qualified Health Plan Certification. As part of our mission to improve access to health care, our letter proposed that CMS consider creating a framework to incorporate health equity measures in the Qualified Health Plan Certification and Network Adequacy Standards. While our response was directed toward a federal comment period, we welcome health plan regulators at all levels to review this framework for addressing the health equity needs of their consumers.
EXORCIZING GHOST NETWORKS
Provider Data Accuracy

No Surprises Act: Provider Directory Verification
ENFORCEMENT GUIDANCE FOR REGULATORS
DISCOVER HOW A DEPARTMENT OF INSURANCE IS USING QUEST ENTERPRISE SERVICES TO AUTOMATE NETWORK REVIEW AND MAKE BETTER-INFORMED DECISIONS REGARDING PUBLIC POLICY.
When the Department of Insurance was using outdated technology to manage its network review processes, it needed a way to streamline the process of monitoring health plans, easily identify areas of insufficient network adequacy for specific specialties, and quickly be able to compare performance between health plans.
By partnering with us, they’re now able to automate their network review process, see provider data in real-time, and compare plan performance—all in one easy-to-use platform. By implementing Quest Enterprise Services, the Department is able to reduce its review time and use the trend data to make better-informed decisions regarding public policy.
If you’d like to learn more about how we can help your department meet its goals, send us a message.