CMS Proposed Rule for CY 2023 Medicare Advantage and Part D

AMEND MA NETWORK ADEQUACY RULES BY REQUIRING A COMPLIANT NETWORK AT APPLICATION Could we be looking at the reinstatement of network adequacy reviews as a condition of initial or service area applications? Possibly. The rule proposes that Medicare Advantage (MA) plan applicants demonstrate they meet the network adequacy requirements for the pending service area before CMS will approve an […]
Improving Network Adequacy and Access For Mental Health

Federal and state policymakers are taking a variety of measures to improve access to mental health services and substance use disorder treatments. Network adequacy and access are prominent areas of such a response directly affecting health plans. This blog post informs stakeholders about the increased emphasis on behavioral health networks and tips on how to […]
FAQs and Provider Directory Requirements: Key Tips and Targets

One of the top questions health insurers have asked us lately is: Will I still need to have a provider directory verification process in place by January 1, 2022? Simply put, yes. In this blog, we’re highlighting the essential points you need to know about the FAQs and provider directory requirements. FAQS ABOUT THE PROVIDER DIRECTORY REQUIREMENTS […]
New Guidance on Provider Directory Verification Requirements Stands Firm on January 1, 2022, Effective Date

In a new guidance document that provided plans and issuers with some enforcement delays over key new price transparency requirements, the Biden administration stood firm on new provider directory verification requirements effective January 1, 2022. BACKGROUND As discussed in a prior post from Quest Analytics, starting on January 1, 2022, section 116 of the Consolidated Appropriations […]
Federal Update: Requirements Related to Surprise Billing; Part 1

On July 1, the Biden administration released an interim final rule with comment period (IFC), “Requirements Related to Surprise Billing; Part I.” This is the first significant step to implementing the No Surprises Act, passed as part of the Consolidated Appropriations Act of 2021 (CAA) in December 2020. The No Surprises Act protects healthcare consumers, […]
Surprises in the No Surprises Act: New Requirements for Plans and Providers Regarding Provider Directory Information

Copyright 2021 Compliance Today, a publication of the Health Care Compliance Association (HCCA). The No Surprises Act was signed into law in December 2020 as part of the massive Consolidated Appropriations Act of 2021.[1] It is the end result of several prior bills that sought to address the national “surprise bill” problem. In recent years, millions […]
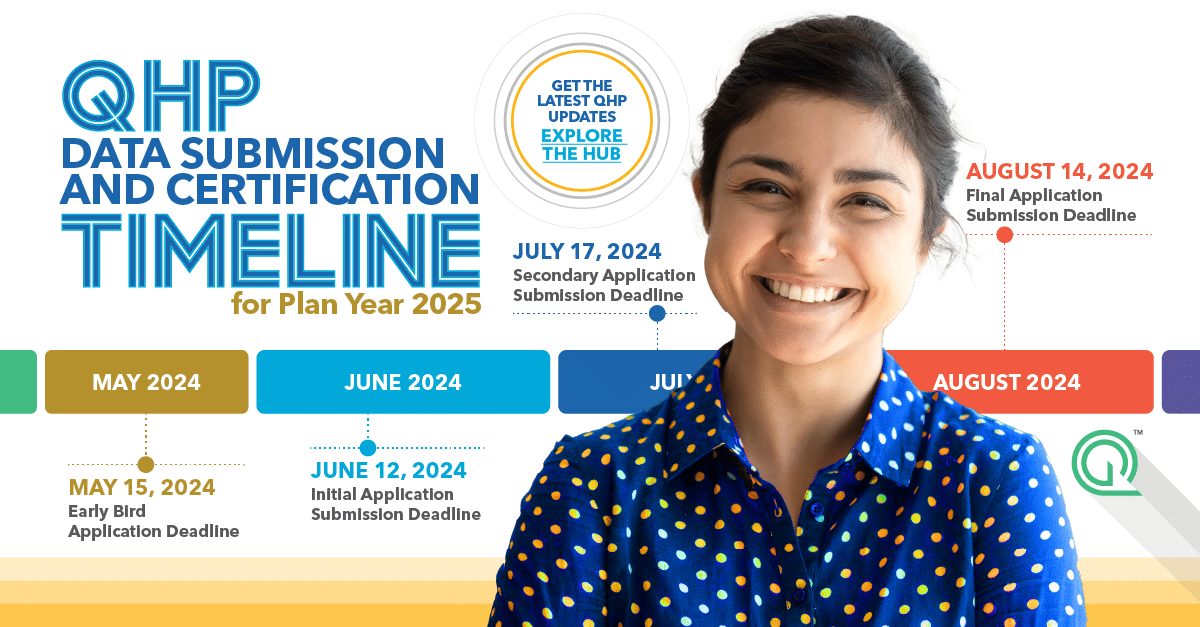
Key Application Dates: Unpacking The CMS Medicare Advantage Calendar
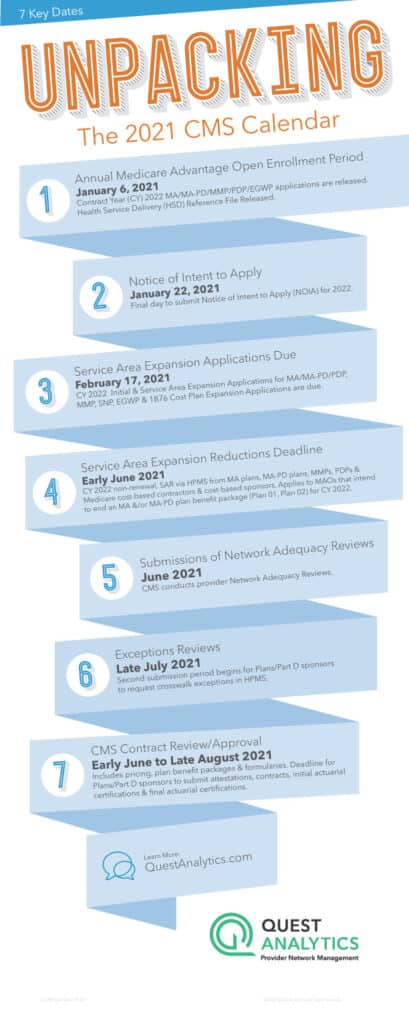
Centers of Medicare & Medicaid Services (CMS) Key Application Dates for CY 2022 Medicare Parts C and D Annual Calendar Our CMS calendar is one of the easiest ways to stay up-to-date with important dates and timelines for CY 2022 Medicare Advantage (MA) plans, Medicare Advantage-Prescription Drug (MA-PD) plans, Prescription Drug Plans (PDPs), Medicare-Medicaid Plans […]
Top 3 Things the “No Surprises Act” Means for Health Plans

It’s staggering to think that, according to researchers, one in five emergency room visits result in an individual receiving a bill for treatment or services they expected to be covered by their health plan, but weren’t. These unexpected, costly, and often frustrating charges are aptly called Surprise Medical Bills. While surprise medical bills impact consumers financially, […]
Insights on Price Transparency: Transparency In Coverage (CMS-9915-F)

On October 29, 2020, the Department of Health and Human Services (HHS), the Department of Labor, and the Department of Treasury released the final version of the Price Transparency Rule. The rule requires most private health plans (self-insured, ERISA), including group health plans and health insurance issuers to publicly disclose the rates they pay healthcare […]
New Metrics are Critical to Addressing Mental Health Access Concerns
Our new normal is far from normal. There is this level of incredible, nonstop uncertainty around our current situation, and none of us are immune. CDC data, collected in late June, noted an increase month-over-month in mental health issues. It showed that 40 percent of adults struggled with anxiety, depression, suicidal thoughts and substance abuse1. […]