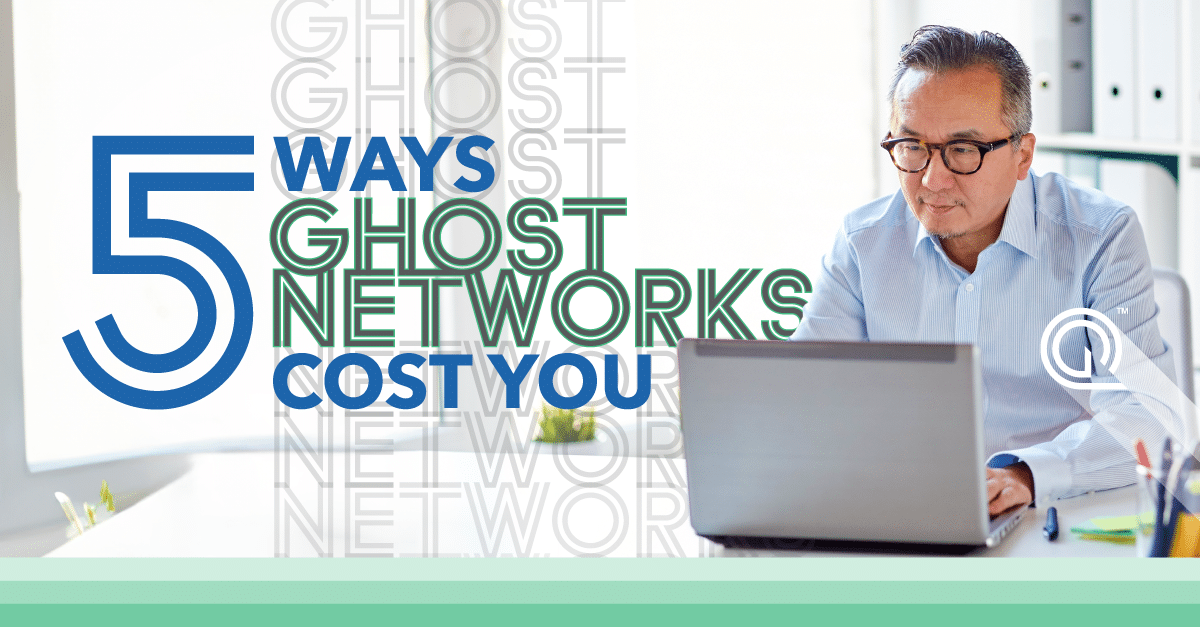
Ghost Networks are a significant challenge in the healthcare industry. By adopting a standard operating procedure that helps you understand which providers are truly clinically active, you can increase the value of your physician network, reduce costs, and improve your ability to deliver high-quality care.
Understanding which doctor or specialist is in-network should be pretty straightforward. But often, that’s not the case. Health, dental, vision, and other insurance databases frequently contain outdated information. As a result, it appears that there are more practitioners, specialists, and other healthcare professionals in-network and available to see patients than actually exist.
This becomes a big problem when that same outdated information is on the insurance website. People who need to make an appointment go there, assuming they have all these choices only to find out that their options have been reduced.
This phenomenon is known as Ghost Networks. If you work with us or follow us, this concern should be no surprise—we’ve been helping clients address it for years. Most recently, we hosted a webinar to discuss the ways we are solving this problem because we believe that aiding consumers who are trying to get care is one of the most important issues out there today.
With the recent surge in attention from the media and health policymakers, we’re sharing our four-phase process to help you avoid the ghost network trap by minimizing inactive providers from your database.
PHASE ONE: AWARENESS
UNDERSTAND WHAT’S AT STAKE
The first phase of the process is crucial for setting the stage for all that comes after it. This is where you will begin to understand what’s at stake and what you need to do to achieve your goals.
First, you need to understand the recent health policy changes that impact you and your business. These are the policies that will have a direct impact on your bottom line, so it’s important that you know exactly how they affect both your business and the industry at large.
Additionally, you want to know the data and metrics required to fully assess the true capacity of the market providers.
After you have gathered the necessary information, assemble the necessary team members and move into the Planning Phase.
PHASE TWO: PLANNING
ESTABLISH PROCESS, STANDARDS AND TOOLS
Let’s talk about taking your ghost prevention strategy from theory to reality. In this phase, you evaluate your current approach to give you a clear idea of what works and what needs to be changed, improved or added.
We recommend you take some time to look at everything from the big picture down to the slightest details. Here are a handful of questions to consider:
- Who works with your provider data?
- What tools do you use for data management, provider verification, network analysis, etc.?
- What tools are you missing?
- Are we working with vendors who can help us achieve our goals?
- What part of your process is automated? What tasks are manual? How much time does each task take to complete? How can you create more time for yourself to focus on other activities?
- How do you measure success? How do you know if you’ve reached your goals or if something needs adjusting along the way?
After answering these questions, it is wise to document your process, standards, and tools.
PHASE THREE: ACTION
DETERMINE THE IMPACT OF REMOVING INACTIVE PROVIDERS
It’s time to start making moves. First, you want to identify which physicians are inactive and remove them from your network or the provider data file you use to analyze your network. Removing ghost providers will improve the quality of care by ensuring that only active providers are available.
Then, you’ll want to assess how removing these providers impacted your network.
The key items to evaluate include:
- How does this impact the depth and breadth of services offered?
- How does it impact the adequacy of the network for payer partners?
- Are there new specialty gaps that you need to close?
- How many active providers do we have? How many inactive providers do we have?
- What are the demographics of these providers? For example, are they male or female? What languages do they speak? Are there any disparities in race/ethnicity or other factors that might impact patient care?
Pro Tip: A quick way to identify if a provider is active is to look at the claims activity.
PHASE FOUR: EXECUTION
Finally, let’s get down to the nitty-gritty and start executing. Here are some tips for how to do just that:
1. Create your plan to curate and optimize your network.
You need to create a clear plan for how you’re going to manage your network, including updating it with new providers and removing providers who are no longer participating in your network. The first step is deciding how often you want to update your network, whether it’s weekly, monthly, quarterly or annually—and then sticking with that timeline.
2. Develop processes and timelines to remove inactive providers.
It’s important to have a process in place for removing inactive providers from your network. You should also determine if there are specific triggers that will cause them to be removed in real-time (e.g., if they’ve been inactive for more than six months).
3. Determine your plan to identify and recruit new physicians.
If there are gaps in coverage in your network due to provider departures or retirements, you’ll want a strategy for finding replacement physicians who can fill those gaps quickly but still provide high-quality care at an affordable price.
Quest Analytics Network Performance Services helps you improve the value of your network by ensuring it is adequate, accurate and ghost-free! Learn More