Policy Trends Across Health Insurance Markets

EVOLVING HEALTHCARE POLICY LANDSCAPE FOR NETWORK ADEQUACY Regulators and policymakers continue to make changes that strengthen federal and state oversight processes for Medicare Advantage, Marketplace, and Medicaid Health Plans. Let’s look at what’s happening in each market. Medicare Advantage: Network Adequacy Requirements for Applications In a previous blog post, we discussed how the Centers for Medicare […]
No Surprises Act Provider Directory Enforcement Guidance for Regulators

Section 116 of the No Surprises Act (NSA) requires health plans to establish a provider directory verification process and a procedure for removing providers or facilities with unverifiable information. No less than once every 90 days, health plans must verify and update their provider directory database. Within 2 business days of receiving a provider update, […]
New Accuracy Rules? New Accuracy Tools

Accuracy Gap Analysis Quest Enterprise Services—QES—has always allowed you to manage provider data accuracy and network adequacy together, which is one of the aspects that sets us apart from other solutions in the industry. Our Accuracy Gap Analysis brings a new capability to the table: It lets you easily see the before and after—what-if scenario—of how […]
What is Provider Data Validation – Are You in Compliance?

WHAT IS PROVIDER DATA VALIDATION? Provider data validation (sometimes referred to as provider data verification or attestation) is a process where health plans confirm each participating provider’s contact and other information displayed in the public provider directory is correct or incorrect. The goal is to update and maintain their provider data to prevent incorrect provider […]
FAQs and Provider Directory Requirements: Key Tips and Targets

One of the top questions health insurers have asked us lately is: Will I still need to have a provider directory verification process in place by January 1, 2022? Simply put, yes. In this blog, we’re highlighting the essential points you need to know about the FAQs and provider directory requirements. FAQS ABOUT THE PROVIDER DIRECTORY REQUIREMENTS […]
New Guidance on Provider Directory Verification Requirements Stands Firm on January 1, 2022, Effective Date

In a new guidance document that provided plans and issuers with some enforcement delays over key new price transparency requirements, the Biden administration stood firm on new provider directory verification requirements effective January 1, 2022. BACKGROUND As discussed in a prior post from Quest Analytics, starting on January 1, 2022, section 116 of the Consolidated Appropriations […]
Federal Update: Requirements Related to Surprise Billing; Part 1

On July 1, the Biden administration released an interim final rule with comment period (IFC), “Requirements Related to Surprise Billing; Part I.” This is the first significant step to implementing the No Surprises Act, passed as part of the Consolidated Appropriations Act of 2021 (CAA) in December 2020. The No Surprises Act protects healthcare consumers, […]
Surprises in the No Surprises Act: New Requirements for Plans and Providers Regarding Provider Directory Information

Copyright 2021 Compliance Today, a publication of the Health Care Compliance Association (HCCA). The No Surprises Act was signed into law in December 2020 as part of the massive Consolidated Appropriations Act of 2021.[1] It is the end result of several prior bills that sought to address the national “surprise bill” problem. In recent years, millions […]
Top 3 Things the “No Surprises Act” Means for Health Plans

It’s staggering to think that, according to researchers, one in five emergency room visits result in an individual receiving a bill for treatment or services they expected to be covered by their health plan, but weren’t. These unexpected, costly, and often frustrating charges are aptly called Surprise Medical Bills. While surprise medical bills impact consumers financially, […]
Designing and Building Clinician Networks That Address Social Determinants of Health
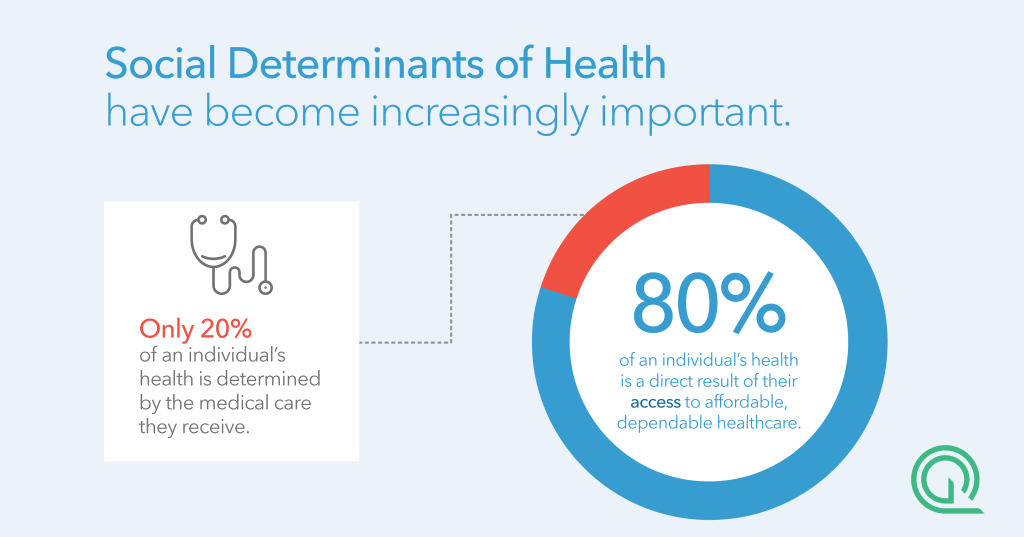
FIVE TAKEAWAYS FROM OUR WEBINAR Watch: Designing and Building Clinician Networks That Address Social Determinants of Health As clinicians and payers take on increasing risk for patient outcomes, it is essential that leaders consider the effectiveness of their networks as well as the accuracy of their clinician directories to ensure they are adequately serving their members. Modern […]