QHP Certification and Network Adequacy Review Timeline
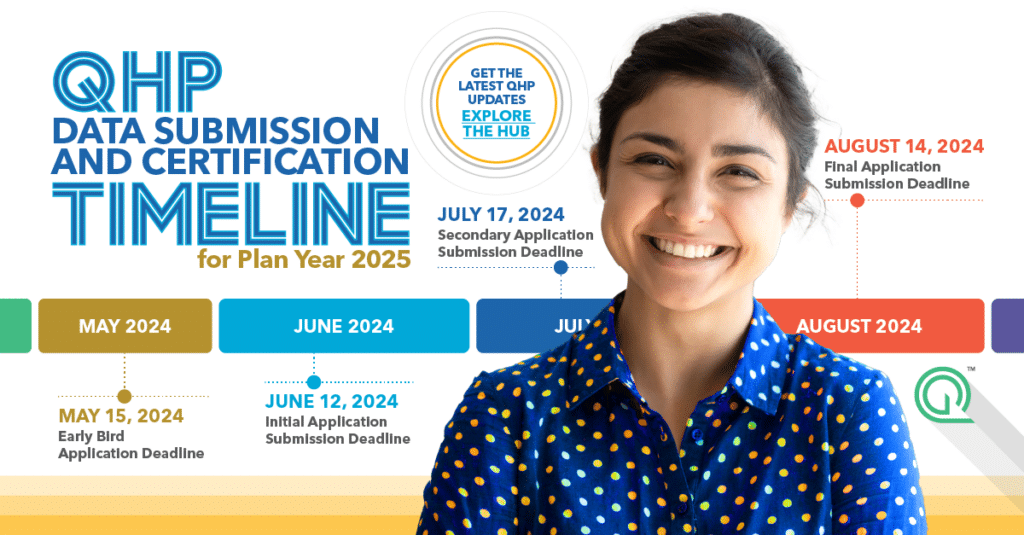
Who doesn’t love a good calendar? We know we do. Whether you’re deep into network adequacy updates or juggling deadlines left and right, we’ve got your back. Our handy calendar lays out the crucial submission dates for Qualified Health Plan (QHP) issuers on Federally-facilitated Exchanges. As a bonus, we’ll keep it updated for you! Go ahead and […]
Understanding CMS Exception Requests for Network Adequacy
Raise your hand if you’ve ever had difficulties meeting network adequacy criteria. Well, you’re not alone. Submitting an exception request for network adequacy involves multiple components, and we’re here to guide you through the process. What is Network Adequacy? Before jumping into exception requests, let’s go over some basics. Medicare Advantage Organizations (MAOs) must comply […]
How Ghost Networks Impact Health Plans and Health Systems
As a health plan or health system, you want to provide the best possible care for your patients. Unfortunately, ghost providers can make this goal difficult to achieve. These non-active providers can harm both patients and your business in numerous ways. Here are five ways ghost networks can cost you, from disrupting access to patient […]
Network Adequacy and Provider Directory Accuracy Policy Updates

Now that 2024 is fully underway, we’d like to bring you up to speed on the network adequacy and provider directory policy updates that emerged between December 2023 and February 2024. Federal Policy Updates CMS Issues Request for Information on Medicare Advantage Data The Centers for Medicare & Medicaid Services (CMS) opened the year with […]
CMS Corrective Action Plans: What Medicare Advantage Organizations Need to Know

The Centers for Medicare & Medicaid Services (CMS) turned things up a notch with new provider directory requirements last year, and now they’re doubling down with Corrective Action Plan requests for Medicare Advantage (MA) Organizations that aren’t playing by the rules. We’re breaking down the latest news about the added provider directory requirements and Corrective […]
Frequently Asked Questions & Answers: Medicare Advantage Applications and Letters of Intent
Medicare Advantage Organizations applying for initial, or service area expansion can use Letters of Intent in place of a signed contract to help meet network adequacy requirements while going through the application process. The intention is to give applicants seeking to expand into a new market the opportunity to reach the threshold for network adequacy […]
CMS Changes the Network Adequacy Application Process for Medicare Advantage Organizations

If you’re involved with compliance, market expansion, or provider recruitment for a Medicare Advantage (MA) Organization, listen up! As organizations seek to either enter the Medicare Advantage market or expand their service areas, understanding these changes is paramount to achieving compliance and securing approval. Network Adequacy Reviews for Initial or Service Area Expansion Applications MA […]
Network Adequacy and Provider Directory Accuracy Policy Updates

What’s the latest news on network adequacy and provider directory accuracy? Here’s what took place in November. Download Article Federal Policy Updates Proposed Rule: 2025 Medicare Advantage Program New Mental Health Facility-Specialty Type and Network Adequacy Exceptions The Centers for Medicare & Medicaid Services (CMS) proposed changes to the Medicare Advantage program for the contract […]
Network Adequacy and Provider Directory Accuracy Policy Updates

Looking for the latest updates on network adequacy and provider directory health policies? You’ve come to the right place. Let’s dive into the latest federal and state policy developments. Download Article Federal Policy Updates Regulators and policymakers are dedicated to strengthening the oversight process for Medicare Advantage, Marketplace, and Medicaid Health Plans, both at the […]
Efficiency on Autopilot: Volume Provider Network Reports and Analytics

What do you think of when you hear the word “report”? Maybe it’s your 5th-grade book report that you poured your heart into. Or perhaps it’s the infamous TPS reports from the movie Office Space. Reports, in general, are not typically associated with excitement. However, within the realm of provider network management, reports are indispensable […]