WE TAKE HEALTHCARE NETWORKS FROM ADEQUATE TO EXCELLENT
POWERING PROVIDER NETWORK MANAGEMENT

WE KNOW YOUR CHALLENGES
Let’s face it, today’s complex regulatory landscape combined with a growing list of new reporting measures like health equity, provider quality, telehealth, surprise billing and social determinants of health can make gaining a competitive advantage seem insurmountable. That’s why Quest Analytics continually evolves with the industry to create the only enterprise solution that brings together real-time provider network adequacy and directory accuracy. Our solutions streamline your organization’s efficiency while simplifying your day-to-day tasks related to provider data management, CMS compliance, market expansion, and provider recruitment.
We know your challenges and have tailored our solutions to help you achieve success.
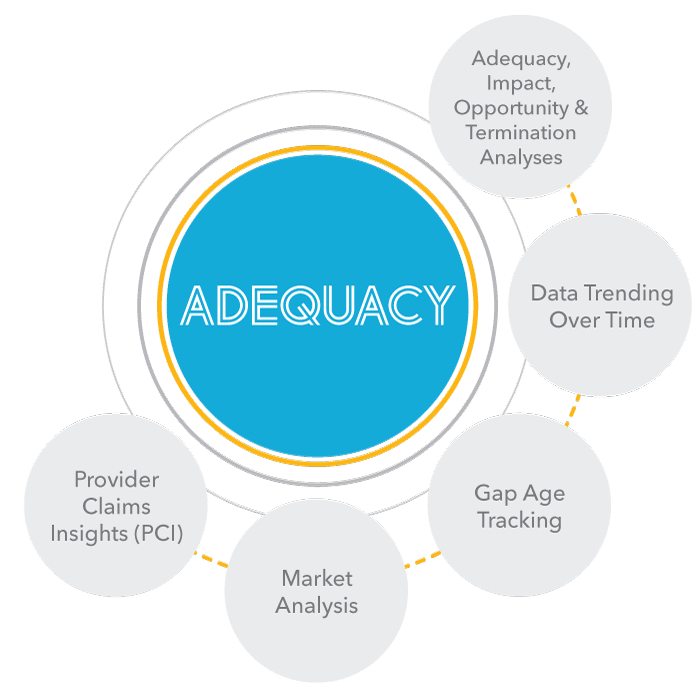
NETWORK ADEQUACY
- How a particular provider could fill or close gaps in your networks.
- How removing a provider impacts your network.
- The level of effort and reward for service area expansion opportunities.
- How including SDoH and telehealth affect your networks.
- The depth, breadth and quality of your networks.
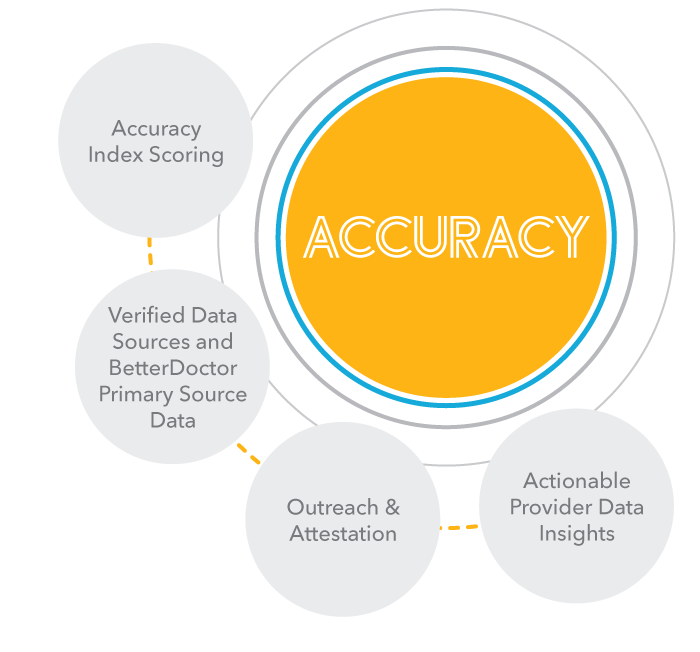
PROVIDER DATA ACCURACY
MEMBER ACCESS
Member access to care is the foundation for maintaining an adequate network and creating competitive advantages. Our Quest Analytics SuiteTM (QASTM) includes features and capabilities that make it easy for you to standardize your data, build access analyses and create maps. You can also use the QAS to assess how competitive your network is through a disruption analysis. As a complement to the QAS, we developed QES Access Reporting. When coupled with our Quest Enterprise Services, you take member access to the next level. It’s the next step into comprehensive access analysis that allows you to see and compare member access with the beneficiary files or your custom membership files. We also provide consulting services to help with regulatory submissions and data management.DELIVER ON TOMORROW’S GOALS BY PLANNING TODAY
We are committed to assisting you in your quest to achieve the Quadruple Aim – lowering costs and ensuring high quality of care while empowering patient and clinician experiences with actionable insights.
Schedule a consultative session with one of our health systems experts to discuss and determine your strategy.